Karen is a breast cancer survivor, a cervical cancer Cervivor and a registered nurse (RN). She shares her unique perspective of being on “both sides” of the healthcare system – as a provider and a patient:

I was working as a nurse when I got “the call” – my gynecologist telling me over the phone that my Pap was abnormal and that I needed to have a biopsy. I didn’t get terribly scared at that time. I knew what a biopsy was. I knew what HPV was. I knew what an abnormal Pap was. “It’s just a biopsy looking for more information,” I’d reassured myself. When the results came back cancer, I wanted to vomit.
The Google “black hole” that even nurses can fall into
Explaining everything to my family was emotionally hard for me. Before I could do that, I personally needed to have a plan, I needed to feel I was in control. I researched nursing school materials, cancer organizations, cancer statistics and treatment plans. I learned early that the last thing anyone with any type of cancer should do is “Google it.”
As a nurse, I had access to quality medical sources. I had credible people I could call. But the lure of Google is strong. As a healthcare provider, I’ve had patients get on blogs and forums and come to me scared by something someone had said – often something that had little to do with their own individual case. Google is a black hole for so many. Even for me at times, even with my nursing training. I’m thankful I had a network of friends who were also nurses to reach out to for information.
The caregiver becomes the patient
As I began treatment, I was able to immediately bond with my oncology provider nurses and the surgery nurses. Many times, however, the care staff had to remind me that I was the patient and to stop trying to do things that I shouldn’t be doing! I’ve heard that doctors are the worst patients. I admit that nurses have got to be too.
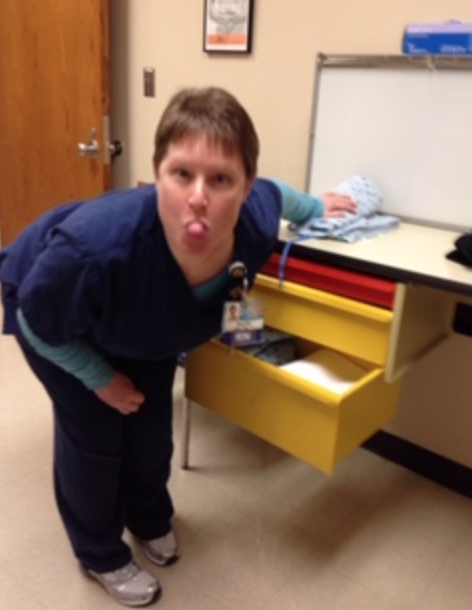
I think because I was a nurse, I tried to be particularly “helpful” when I was in the hospital receiving care. Having worked with residents and medical students before, I was very open to them watching and asking questions. I often told residents and medical staff in training that they can ask me anything, they just need to know that I don’t have a filter when I answer. I tell them the down and dirty truth!
As a nurse, not being in the position of caregiver can be a challenge. Many times nurses will put their own personal needs behind everyone else. So having my family and friends take care of me warmed my heart. Going through radiation and chemo treatment was difficult. I had nausea after chemotherapy (I can’t even look at a Goldfish cracker anymore). I had muscle spasms and diarrhea (I called it “liquid death”). My family and friends taking care of me showed me their love. There is a saying “what you give, you can get back tenfold.” I definitely felt swaddled in love. They even organized a fundraiser to help me with my expenses.
The endurance challenge of returning to nursing after cancer treatments
The first part of July 2016, I returned to my nursing job. I think this is one of the hardest jobs to return to after cancer because of the time on your feet and the endurance needed. What normally only took me 15 minutes would take me an hour to complete. My legs felt like I had concrete in my shoes. I needed to be able to go to the bathroom at a moment’s notice because of diarrhea and bladder issues. My body hurt everywhere. I had panic attacks that were debilitating. I felt guilty because I knew I wasn’t holding up to my standards of care. There were many times that I worried that I would make mistakes. There were also several times that my charting was done late because I couldn’t get to it with everything else going on. The best analogy that I can think of is “this is like running a marathon on crutches.”
Ultimately, I had to leave my job. I fell into a dark pit of depression and anxiety.
The past few years since my cervical cancer treatments have been rough. I’ve had to have repeated biopsies because of abnormal Pap results. I’ve seen a gastroenterologist, a urologist, and an orthopedic doctor along with my psychiatrist and counselor. I’ve been diagnosed with radiation colitis that causes me severe abdominal pain and diarrhea. I’ve had to have my hip replaced because of a tear in the cartilage that wasn’t repairable due to the radiation. My depression and panic attacks are still debilitating. I also have been diagnosed with lymphedema of my right leg. I have to elevate my legs four times a day for 40 minutes – above my head, mind you! I also have to wear compression hose and hook up to a machine that pushes the fluid out of my leg every night.
These days I’m working at keeping my head together. It’s one day at a time, and sometimes, one minute at a time. With the help of my family, friends, medical teams, and my Cervivor community, I’m surviving.
Educating doctors and nurses about cervical cancer prevention
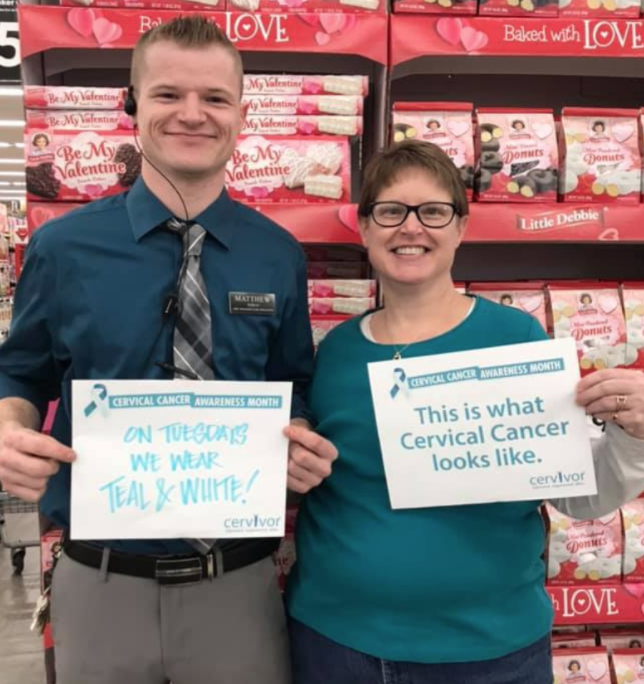
With the help of Cervivor and my training at Cervivor School, my goals now are to educate and advocate to general practitioners that they need to discuss HPV immunizations with every patient, no matter their age or sex.
My goal is to promote education to medical providers so that they will in turn educate their patients and friends on HPV prevention and the importance of the annual women’s health exam. I reach out to medical schools to connect with medical students and residents. I want to share my story with them, have them hear what I went through as both a nurse and a patient, and encourage them to be more proactive when it comes to cancer screening and prevention. I think being a nurse and speaking to them as a nurse and not just a patient can be particularly powerful.
Also, because of my nursing training I can be an effective communicator about HPV immunization and screening and will convey information in a way that people will understand. Like, when you talk about there being more than 400 different strains of HPV, only some of which can cause a cancer. I can relate it to different strains of the flu or the cold, so that people can grasp a little bit better idea of it.
I am proud to say that I am a Cervivor Ambassador. My Cervivor school training has offered me the tools and understanding of how to listen to others’ questions and concerns and how to encourage them to talk to their providers about Pap testing, HPV testing and HPV vaccination.
After all, If you don’t ask, your provider can’t answer.

Karen North lives in Liberty, Missouri. She is a retired registered nurse. Her world is her family, fur-babies, and friends. As of the writing of this blog post in 2020, she is a six-year breast cancer survivor and a, come June, four-year cervical cancer survivor.
Read Karen’s Cervivor story.
Read Karen’s blog post on being both a breast cancer survivor and cervical cancer Cervivor.