We in the Cervivor community understand and appreciate that the human papillomavirus (HPV) vaccine is a cancer vaccine. The word’s first cancer vaccine, in fact. We understand that it can save lives. Yet, misconceptions and “fake news” about the HPV vaccine persist. The myths and misconceptions have obscured the importance of the vaccine for cancer prevention – for both men and women.
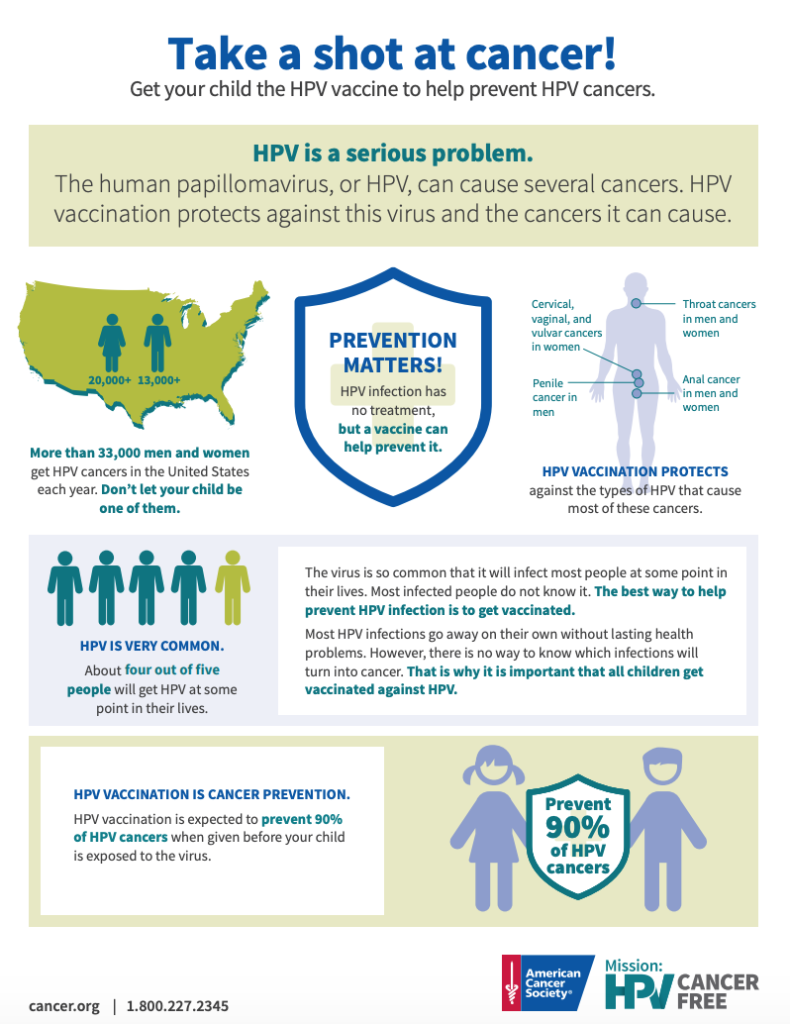
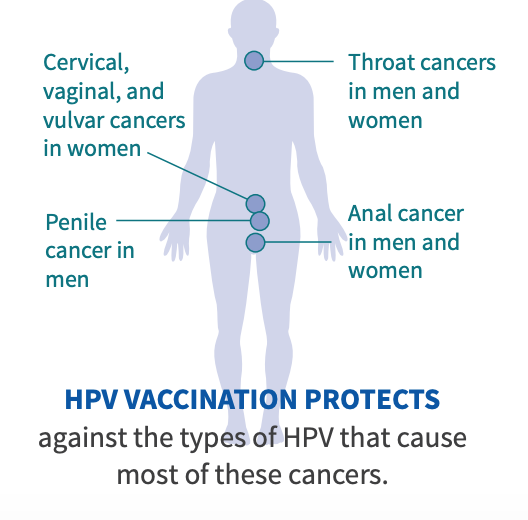
The more parents who take their children to get vaccinated, the broader the adoption across the population, the closer we will get to our goal of ending cervical cancer – as well as other cancers related to HPV, including penile, anal, vaginal, vulvar and throat cancers.
MYTH 1: HPV vaccination is not safe.
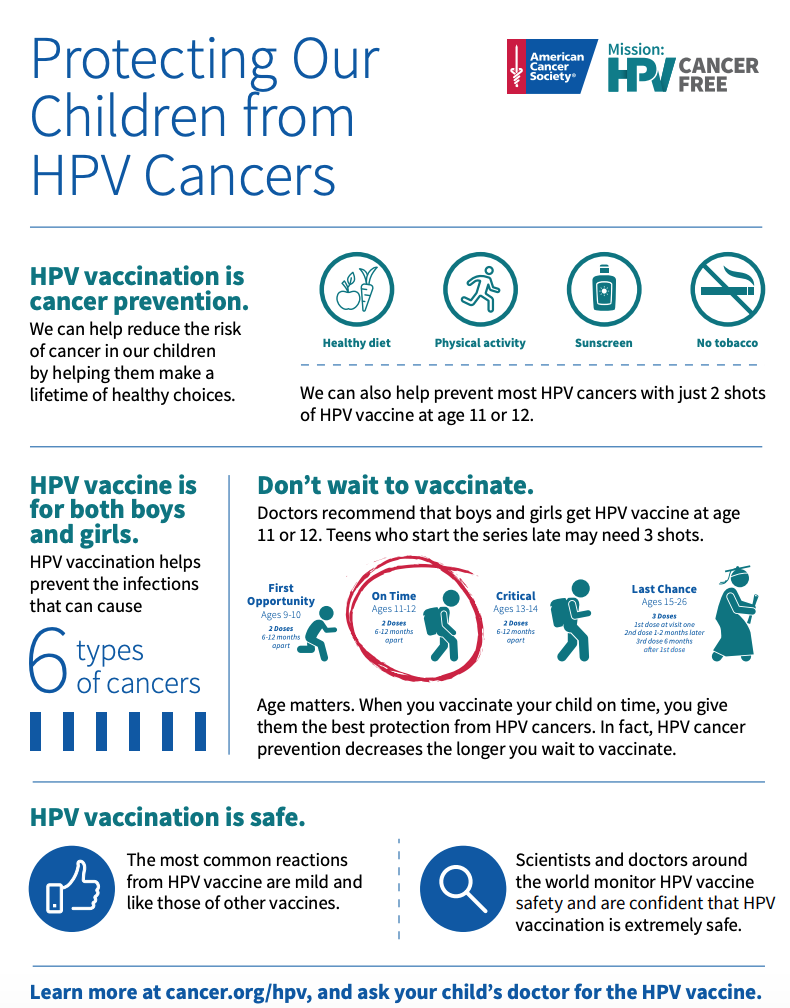
FACT: The HPV vaccine is safe and doesn’t contribute to any serious health issues. The vaccine itself has been researched for many years (including 10+ years of research before it could even be used in humans) and has been approved by the Food and Drug Administration since 2006. Similarly, the Global Advisory Committee on Vaccine Safety of the World Health Organization annually reviews all published and emerging data about the vaccines in real-world use and has, year after year, declared HPV vaccines safe for use.
MYTH 2: The HPV vaccine has side effects.
FACT: The HPV vaccine has the same potential side effects as any other vaccine: pain or redness at injection site, nausea, and headaches – all of which are temporary. These are minor effects or drawbacks especially when compared to all of the benefits you gain from the vaccine in the long run: protection against HPV-related cancers. Rarely, an allergic reaction to a vaccine component or ingredient can occur – but that is true of all vaccines and medicines. All people are monitored for 15 minutes after having the vaccine. If an allergic reaction does occur, it can be treated quickly – as immunization providers are trained to deal with such a reaction. Again, this can happen with ANY vaccine and is not specific to the HPV vaccine.
MYTH 3: Only girls need to get the HPV vaccine; boys don’t need it.
FACT: HPV vaccines are approved by the U.S. Food and Drug Administration for males and females ages 9 to 45. HPV affects both men and women. In men, HPV can cause penile, anal and oral cancer. In women, HPV is not only the cause of cervical cancer, but is also associated with some vaginal, vulvar, anal and throat cancers. The HPV vaccine can protect against these cancers, as well as protect against genital warts (which are also associated with HPV). So the vaccine truly can help both sexes. Overall, the vaccine will have quicker, greater impact and protect more people if both girls and boys get vaccinated. The ideal time to vaccinate is in the tween and early teen years. Research shows that younger people create more antibodies to the vaccine than those aged in their late teens. (This is why those aged 14 and under usually only need two doses instead of the three doses administered to adults.)
MYTH 4: Since the HPV vaccine is not required in every state, it’s really not important.
FACT: While the HPV vaccine is not mandatory in some states, this could soon be changing. More and more states are now requiring that kids be immunized. Many have programs to fund HPV vaccination, even if it is not a state requirement. Regardless of whether or not a state has laws or regulations about the HPV vaccine put in place, it is still a highly important cancer vaccine for children to receive. HPV causes virtually all cases of cervical cancer, as is also associated with vulvar, vaginal cancers, penile cancers, anal and oral cancers. Vaccinating tweens and teens against HPV is a major step to help protect them from these deadly cancers.
MYTH 5: Getting the HPV vaccine will encourage adolescents to be more sexually promiscuous.
FACT: Research has shown that there is no evidence that boys and girls who receive the vaccine have sex earlier than those who don’t have the vaccine. Nor do they have more sexual partners once they became sexually active. No research links the HPV vaccine to increases in sexual activity.
MYTH 6: Only sexually active people need protection against HPV.
FACT: The vaccine is most effective when administered to individuals who have not been exposed to HPV. Thus, giving the vaccine to tweens and teenagers before they become sexually active, offers the best protection. However, the vaccine is recommended in individuals who are sexually active as well. The HPV vaccine is approved by the FDA to be given to males and females as early as age 9 and up to age 45
MYTH 7: You got the HPV vaccine, so you can skip your Pap test.
FACT: Women who have been vaccinated against HPV should still keep up with cervical cancer screenings. As with any vaccine, the HPV vaccine may not fully protect everyone who is vaccinated and does not protect against all HPV types. Nor can the vaccine help clear an HPV infection that is existing in the cervix at time of administration. While the frequency of Pap testing can be extended for women who have been vaccinated because of the protection afforded by the vaccine, annual health visits should be continued together with the many other important health checks that occur at those visits.
Resources to Share
The American Cancer Society has several downloadable, printable graphics and handouts focused specifically on HPV vaccination.