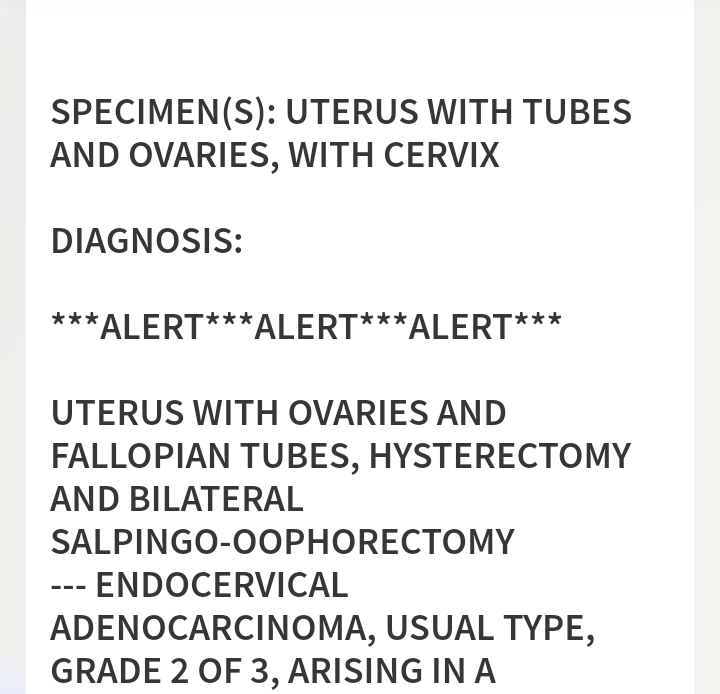
On May 26, 2017 I found out my entire reproductive system needed to be removed when I received a cancer diagnosis over the phone: grade one endometrial cancer. The gynecologist said I would receive a call from oncology that day and that they were deeply sorry. One week prior, I’d received an acceptance letter into the accelerated MSW program. The start of that semester was not to be. I had hopes to begin the following cohort.
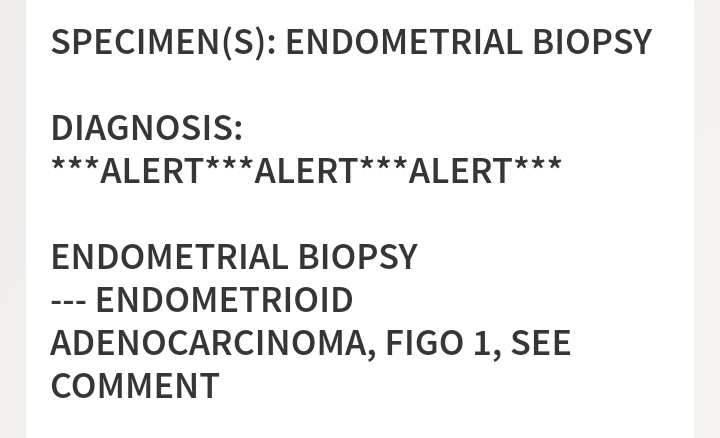
I was wheeled into surgery in July, eyes still damp from tears. Within a week of surgery, I received news that my grade one endometrial cancer was instead invasive grade two cervical cancer. Oncology apologized for the unexpected diagnosis. The tumor board suggested daily high dose pelvic radiation with concurrent weekly platinum chemo. I stood up, holding my entire post-surgery swollen abdomen and pelvis, agreed to it all, and left. I called my master’s advisor and said the treatment would continue through the beginning of winter. I found it difficult to breathe and I couldn’t hear what she said, except that she was terribly sorry. It wasn’t just the additional news of the treatment. It was the news coupled with the fact that I had already lost so much prior to this. I’d just spent a week in the hospital before my diagnosis due to severe asthma attack and had to rebuild my lungs. I had put myself through school for all my previous degrees (summa cum laude with my most recent), while co-managing a department and staff, while supporting my household which we lost to foreclosure after my partner lost his job (packing instead of going on a honeymoon) and staying with my mom months at a time to care for her after each of her falls.
I continued to focus on my dreams, even after my department closed to a college-wide restructure, my health deteriorated, and I lost my mother. The MSW dream wasn’t meant to be, and it was the first time in my life I couldn’t make the impossible possible for myself. I did not tolerate treatment well. In fact, the following years were spent dealing with the fallout from the radiation and now small nerve neuropathy from the cisplatin. Still, during this time, I became a cervical cancer advocate. Word got out, and I would begin to receive calls from strangers whose loved ones were at end of life. I would hold the hands of the dying after driving to their homes and hospitals. I used my adult-ed teaching and training to raise awareness and educate the community about cervical cancer.

There is more on the horizon that only those closest to me know about. I am also due to have another major surgery to my abdomen soon and the level of fear is exquisite. Through everything, I am still grateful knowing that I find beauty in the lakes and the trees. Comforted, that I am a part of a community of survivors who hold space for each other. Although my actual cancerversary is November 1, the day I completed treatment, this month I remember the three words that changed my quality of life forever.
Lorie is a three and half year cervical cancer survivor, thanks to life-changing surgery and cancer treatment. Prior to her diagnosis, Lorie worked in research, employee training and development, case management, workshop facilitating and sales. She now dedicates herself to cancer advocacy and support, community education on cancer and HPV awareness as well as elder and animal rights. Lorie is a community member of Cervivor.