By Kyle Minnis, Cervivor Communications Assistant

September is more than just Gynecologic Cancer Awareness Month (GCAM)—it’s a call to action for anyone affected by the five “below-the-belt” cancers—cervical, ovarian, uterine, vaginal, and vulvar. Patients, survivors, caregivers, advocates, experts, and others come together to share this critical, life-saving knowledge: Greater awareness of risk factors, prevention, and early symptoms could mean fewer diagnoses and more birthdays for thousands of people each year. In 2025, the American Cancer Society (ACS) estimates that more than 119,000 Americans will be diagnosed with gynecological cancer, and roughly 34,630 will die from these diseases.

“Gynecologic cancers can impact people of all ages and ethnicities, and there is incredible need for awareness,” says Mayo Clinic radiation oncologist Dr. Allison E. Garda, M.D., who lists the cancers in decreasing order of incidence, according to the national Surveillance, Epidemiology, and End Results (SEER) Program‘s 2025 estimates: uterine (69,120), ovarian (20,890), cervical (13,360), vulvar (7,480), and vaginal (5,550).
Collectively, these cancers are a growing public health challenge—one that Cervivor is committed to reversing year-round, not just during GCAM. Consider these facts about gynecologic cancers:
- HPV vaccination could prevent almost all cervical and many vaginal and vulvar cancers. Regular screening—such as Pap tests to detect precancerous cell changes and HPV tests to identify the virus responsible—has been proven to significantly reduce fatalities through early intervention. However, childhood vaccination rates are declining nationwide, and too many barriers to preventive care still exist.
- Uterine cancer incidence and mortality are climbing in the U.S., with age-adjusted death rates rising by around 1.6% per year between 2014 and 2023, according SEER. This increase is fueled by rising rates of obesity and metabolic conditions—known risk factors that can be monitored and managed through preventative care.
- Despite recent advances, ovarian cancer’s prognosis remains poor, especially when diagnosed at later stages. SEER reports that the relative five-year survival rate is just 51.6%—compared to 91.7% for breast cancer and 68% for cervical cancer. Early symptoms are subtle, and too few cases are detected at an early stage.
- Even after survival, many live with long-term pelvic health issues and quality-of-life challenges that too often go untreated.
For all these reasons and more, it’s vital to break the silence, raise awareness, and advocate for those affected by gynecologic cancers—while also listening to survivors as they share their lived experiences. Understanding your gynecologic health is the first step toward prevention, so let’s start with the basics.
Gynecologic Cancer Awareness: Understanding Types, Risk Factors, Symptoms, and Treatments
Gynecologic cancers are united by their location—the female reproductive system—but are unique in their behavior. While some symptoms may overlap, every type presents its own challenges. Here’s an overview of gynecologic cancer facts to help you understand the barriers to prevention, early detection, and better outcomes—because knowledge is power when it comes to your health.
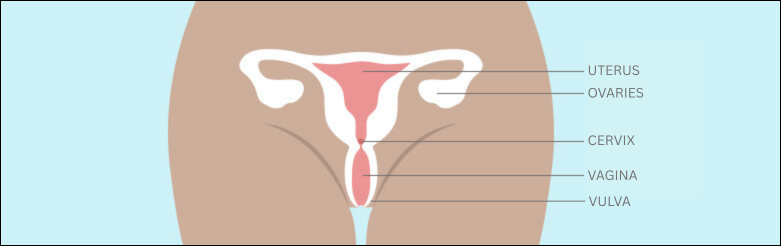
Where Different Types of Gynecologic Cancers Form
- Uterine (Endometrial) Cancer begins in the endometrium, the inner lining of the uterus. This tissue is highly responsive to hormonal changes, which is why uterine cancer is closely linked to factors that affect hormone levels, like obesity and metabolic conditions.
- Ovarian Cancer starts in the ovaries, with most cases thought to originate in the cells on the ovary’s outer surface.
- Cervical Cancer arises in the cervix, linked directly to HPV infection, and can be detected early through screening.
- Vaginal Cancer begins in the tissues of the vagina and is strongly associated with HPV infection.
- Vulvar Cancer develops on the outer surface of the female genitalia, often affecting the labia. It is also linked to HPV as well as lichen sclerosus and other chronic vulvar conditions.
Key Risk Factors for Gynecologic Cancers
Different gynecologic cancers have unique drivers, yet several key risk factors overlap. Here are the most common:
- HPV Infection: Human papillomavirus (HPV) is one of the world’s most common viruses and causes multiple gynecologic cancers—cervical, vaginal, and vulvar—and others like anal, throat, and penile cancers. Persistent infection with high-risk strains can trigger precancerous changes and, if untreated, develop into cancer. “We are seeing more HPV-driven vulvar cancers affecting younger patients,” notes Dr. Garda. Hear from this vulvar cancer survivor.
- Family History of Cancer: Genetics also plays a role. Roughly 10 to 15% of ovarian cancers and 5% of endometrial cancers are hereditary, often tied to BRCA1/2 or Lynch syndrome, reports OncoLink.
- Aging: According to the National Cancer Institute (NCI), getting older is the single greatest risk factor for cancer overall—and especially for some gynecologic cancers: The median age of diagnosis is 64 for uterine cancer and 63 for ovarian cancer, reports SEER.
- Obesity: The Centers for Disease Control and Prevention (CDC) includes both uterine and ovarian cancers among the 13 cancers linked to obesity, which now affects more than 40% of Americans. The ACS notes that about 57% of endometrial cancers are tied to excess weight, and severe obesity (BMI ≥ 40) can raise risk by up to sevenfold compared with a healthy weight.
- Metabolic Conditions: Diabetes and metabolic syndrome can increase the risk of uterine and ovarian cancers. Having three or more metabolic syndrome components (e.g., high blood sugar, hypertension, obesity) increases uterine cancer risk by more than three times, according to the ACS’s Cancer journal last year. Diabetes alone raises ovarian cancer risk by about 17%, according to 2023 research.

Even if you have risk factors, don’t feel discouraged or hopeless—or internalize shame or blame. Cervivor supporter Mechal Haas, who was diagnosed in 2022 at 45 with both endometrial and ovarian cancer, reflects: “At first I blamed my weight and not prioritizing self-care, but I’ve learned that women at healthier weights who exercise regularly are also diagnosed with these cancers. Since there’s no early detection test for ovarian cancer, know the symptoms, find a doctor you trust, get regular check ups, and advocate for yourself.”
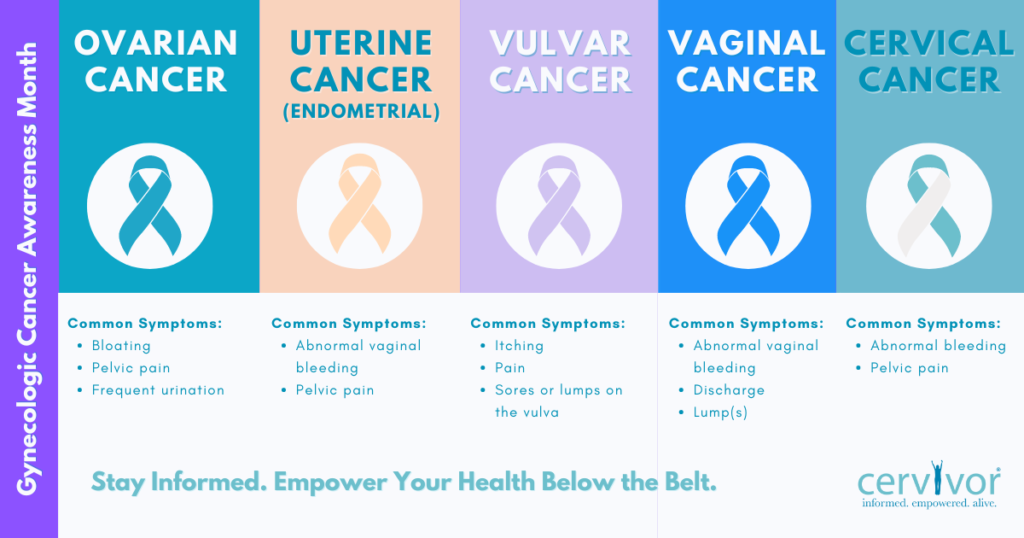
Common Gynecologic Cancer Symptoms
“Symptoms may sometimes be obvious—such as vaginal bleeding or discharge—or more subtle, like pelvic or abdominal pain, bloating, nausea, appetite changes, or shifts in bowel or bladder habits,” explains Dr. Garda. Too often, these signs are dismissed as “normal aging” or mistaken for conditions such as fibroids, Polycystic Ovary Syndrome (PCOS), or endometriosis.
Early detection saves lives—especially for cervical and uterine cancers, which are often highly treatable when caught early. Being aware of these symptoms is crucial for maintaining your gynecologic health. Here are ones to watch for:
- Abnormal vaginal bleeding or discharge — cervical, uterine, ovarian, and vaginal cancers
- Pelvic pain or pressure — uterine and ovarian cancers
- Pain or bleeding during intercourse — cervical and vaginal cancers
- Feeling full quickly, bloating, or abdominal/back pain — ovarian cancer
- Changes in urination or bowel habits — ovarian and vaginal cancers
- Vulvar itching, burning, pain, or skin changes — vulvar cancer
For Cervivor community member Erica Lopez, a history of gynecologic issues led her to dismiss what were actually cancer symptoms. “I always bled heavily and with clots, but over time, my clots started getting bigger, and bleeding got worse. I thought it was my PCOS… I was fatigued, but I’ve always had anemia,” recalls the Bronx mother, who was diagnosed in 2022 at 34 with stage 3 cervical cancer. “When the pain during intercourse and heavy clots started, I knew something was wrong, but I waited. If I’d listened to my body, maybe I wouldn’t have been on such a high stage.” Today, she urges, “Ladies, always check yourselves for symptoms, even if you’re afraid of the outcome.”
Others may delay seeking care for different reasons, including past trauma. Cervivor community member MaShell Moore-Felks shares how being molested as a teen, experiencing years of irregular bleeding, and enduring two miscarriages—including one just a week before her son’s due date—made it difficult to understand her confusing symptoms or recognize their urgency.
“In 2012, I was treated for PCOS. The following year, I was diagnosed with endometriosis and tried various hormonal medications, including pills and the Mirena IUD. In 2015, I had it replaced; in 2017, I had it removed completely. After bleeding for another whole year, I was diagnosed with cervical cancer in 2018,” recalls the Mississippi mother, adding, “Looking back, I believe I was misdiagnosed at several points along the way, and there is more than one responsible party.”


Types of Treatments for Gynecologic Cancers
Treatment for gynecologic cancers depends on the cancer type, stage, location, and the patient’s overall health, and fertility goals. They generally fall into three main categories—surgery, radiation therapy, and chemotherapy—and patients often receive a combination of these approaches.
- Surgery: Surgery, the most common treatment for gynecologic cancers, involves removing cancerous tissue. Options range from fertility-sparing procedures to extensive operations, including:
- Hysterectomy: The most common non-obstetric surgery in the U.S., with roughly 600,000 performed annually, it can remove the uterus alone or also the cervix, ovaries, and fallopian tubes. While most are done for benign conditions, hysterectomies can be life-saving for uterine cancer and certain cervical cancers.
- Oophorectomy: A common treatment for ovarian cancer, this surgery removes one or both ovaries and is often performed alongside the removal of the fallopian tubes.
- Trachelectomy: This fertility-sparing surgery removes the cervix and surrounding tissue while leaving the uterus intact, typically for early-stage cervical cancer.
- LEEP or Cone Biopsy: For very early-stage cervical cancer, LEEP (Loop Electrosurgical Excision Procedure) and cone biopsy remove precancerous or early cancer cells from the cervix.
- Debulking Surgery: Common in ovarian cancer, this surgery removes as much tumor as possible before chemotherapy, improving treatment effectiveness.
- Hysterectomy: The most common non-obstetric surgery in the U.S., with roughly 600,000 performed annually, it can remove the uterus alone or also the cervix, ovaries, and fallopian tubes. While most are done for benign conditions, hysterectomies can be life-saving for uterine cancer and certain cervical cancers.
- Radiation Therapy: This treatment uses high-energy rays to destroy cancer cells, and can be delivered externally or internally (brachytherapy), placing radioactive sources directly near or inside the tumor. Internal radiation can be intensive—MaShell recalls the “brutal” treatments involving hot “irons” placed inside her pelvis.
- Chemotherapy: “Chemo” involves powerful drugs that target cancer cells throughout the body. These drugs may be administered alone or alongside surgery and/or radiation. It can be given before surgery to shrink tumors, after surgery to eliminate remaining cells, or in advanced cancers to control progression.
Shared Health Challenges for Gynecologic Cancer Survivors
Undergoing treatment for gynecologic cancers can be life-saving—but for many survivors, “ringing the bell” after finishing that last treatment marks the beginning of a new chapter filled with lasting physical, emotional, and sexual health challenges. Common concerns include:
- Surgical Menopause: Hysterectomies can trigger sudden surgical menopause, bringing hot flashes, mood changes, and long-term hormonal effects. Later, many survivors experience natural menopause on top of these changes, which can amplify physical and emotional challenges.
- Pelvic Health Issues: “Surgery, radiation, and hormone therapy can cause vaginal shortening, tissue tightening, and other pelvic floor issues, which can significantly impact quality of life,” says Dr. Trisha McCulloch, DPT, a pelvic rehabilitation expert with The University of Kansas Health System. Survivors often face:
- Incontinence and Bowel Changes: Up to 76% of gynecologic cancer survivors experience urinary incontinence, and bowel changes are common—all far higher than in the general population. “Even seven years later, my bladder issues persist,” shares MaShell.
- Painful Intercourse and Intimacy Difficulties: Nearly 60% of survivors report painful intercourse after treatment. These challenges often compound emotional and relational stress. Read about gynecologic cancer survivors’ setbacks and successes navigating intimacy.
- Incontinence and Bowel Changes: Up to 76% of gynecologic cancer survivors experience urinary incontinence, and bowel changes are common—all far higher than in the general population. “Even seven years later, my bladder issues persist,” shares MaShell.
- Infertility: Depending on the treatment, fertility can be significantly affected, particularly after hysterectomies, ovarian removal, or aggressive cervical procedures. Learn more about the infertility struggles faced by gynecological cancer survivors who’ve become powerful advocates.
- Mental Health Struggles: Depression, anxiety, brain fog, and post-traumatic stress are common among all cancer survivors. Because “below-the-belt” cancers are often stigmatized or kept private, gynecologic cancer survivors may experience intensified isolation, shame, and stress.
MaShell is candid about her ongoing challenges: “My mental status fluctuates throughout every single day.” For Mechal, who says she’d always wanted children, infertility can trigger difficult emotions during community and family milestones. “Birthdays, graduations, first day of school, and other celebrations can be hard because I don’t have kids,” she shares. Find out how other survivors deal with similar mental health challenges.
Support for Gynecologic Cancer Survivors
Gynecologic cancers share many similarities—from risk factors and symptoms to treatments and survivorship struggles. The healing journey requires a holistic approach that supports physical, emotional, and social well-being. Strong support networks and resources are vital, and survivors often find ways to reclaim their life, identity, gynecologic health, and vitality through strategies such as:
Finding Your Community
Support networks like Cervivor provide understanding and connection that extend beyond the clinical setting—and that “we get it” experience can make all the difference.
As Erica shares, “Being a part of the Cervivor community helped me understand I wasn’t going through this alone.” For Mechal, engaging with Cervivor and other advocacy groups has been an important part of her healing. “Through the Foundation for Women’s Cancer, Cervivor conferences, HPV awareness events, and Society of Gynecologic Oncology (SGO) patient meetings, I’ve connected with incredible gynecologic cancer survivors whose advocacy inspires me every day.”
To keep the community support, inspiration, and advocacy going, Cervivor is hosting a free webinar—GCAM 2025 Power Hour: Stories, Science & Action—on September 25, 2025, at 7 p.m. EST. Register now to join this unique opportunity to hear personal survivor stories, learn the latest science, and discover ways to take action.
Pelvic Health Therapy

Recovery looks different for every survivor, yet pelvic floor therapy—a type of rehabilitation that strengthens and restores the muscles of the pelvic region—is often overlooked in follow-up care. It can reduce pain and anxiety, improve sexual health, and help survivors regain confidence, fostering greater independence and overall life satisfaction.
The pace of recovery depends on the aggressiveness of the cancer and the treatments received. Pelvic rehab expert Dr. McCulloch encourages survivors to share their symptoms openly. “Being grateful for survival doesn’t mean you should ignore ongoing challenges or compare yourself to others,” says Dr. McCulloch, who will be part of the expert panel for Cervivor’s upcoming webinar. “Feel empowered to ask questions, communicate your symptoms, and advocate for yourself—not just to survive, but to truly thrive.”
Sharing Your Story
Telling your gynecologic cancer survivor story creates purpose, connection, and helps break the stigma and silence around these cancers. By speaking up, survivors empower others to seek care, recognize symptoms, and know they’re not alone. Mechal has experienced these benefits firsthand: “As a patient advocate, I’ve seen how powerful personal stories can be in raising awareness, shaping policy, and motivating action.” Submit your Cervivor Story to make an indelible impact—like hundreds already have—and share it with your community.
Ultimately, a gynecologic cancer diagnosis and treatment don’t have to be faced in silence. By talking openly about symptoms, sharing survivorship experiences, and advocating for comprehensive care—this Gynecologic Cancer Awareness Month and every month—we can protect lives and support the mothers, grandmothers, aunties, sisters, daughters, and friends in our communities.
If you found this blog post helpful, please share it with friends or family members. You may just save a life. Questions? Contact us at [email protected].
About the Author

Kyle Minnis is a senior studying Strategic Communications at the University of Kansas. He is currently serving as Cervivor’s Communications Assistant.