On Saturday, the cancer community came together to share a unified message: Cancer Can Go Fly a Kite! And it was nothing short of amazing! There were so many beautiful photos, videos, and virtual kites shared. It reminded us of one very important message, we are always stronger together.

Read the Kickoff Message from Our Founder, Tamika Felder.
Cancer Can Go Fly a Kite!
Cancer Screenings: We want others to understand, the global pandemic put a dramatic halt on cancer screening rates and cancer diagnoses. Though rates are climbing back up, they are still not at pre-pandemic levels and it’s a problem. We know that prevention and early detection saves lives.
Have you scheduled your cancer screenings yet? Stay up-to-date on age and risk appropriate guidelines by speaking with your doctor and utilizing the American Cancer Society’s Quick Reference Guide.
Caregivers: Support those who support you. Caregivers deal with so much when a loved one is diagnosed with cancer that they often forget they need support too. We are so grateful for the caregivers in our community.
Community: Cancer can feel isolating and it can make you feel lonely but when you find your community, it can make things feel less scary. The Fort Independence Warriors in New York know all about the word community. They showed up loud and proud for #CCGFAK.

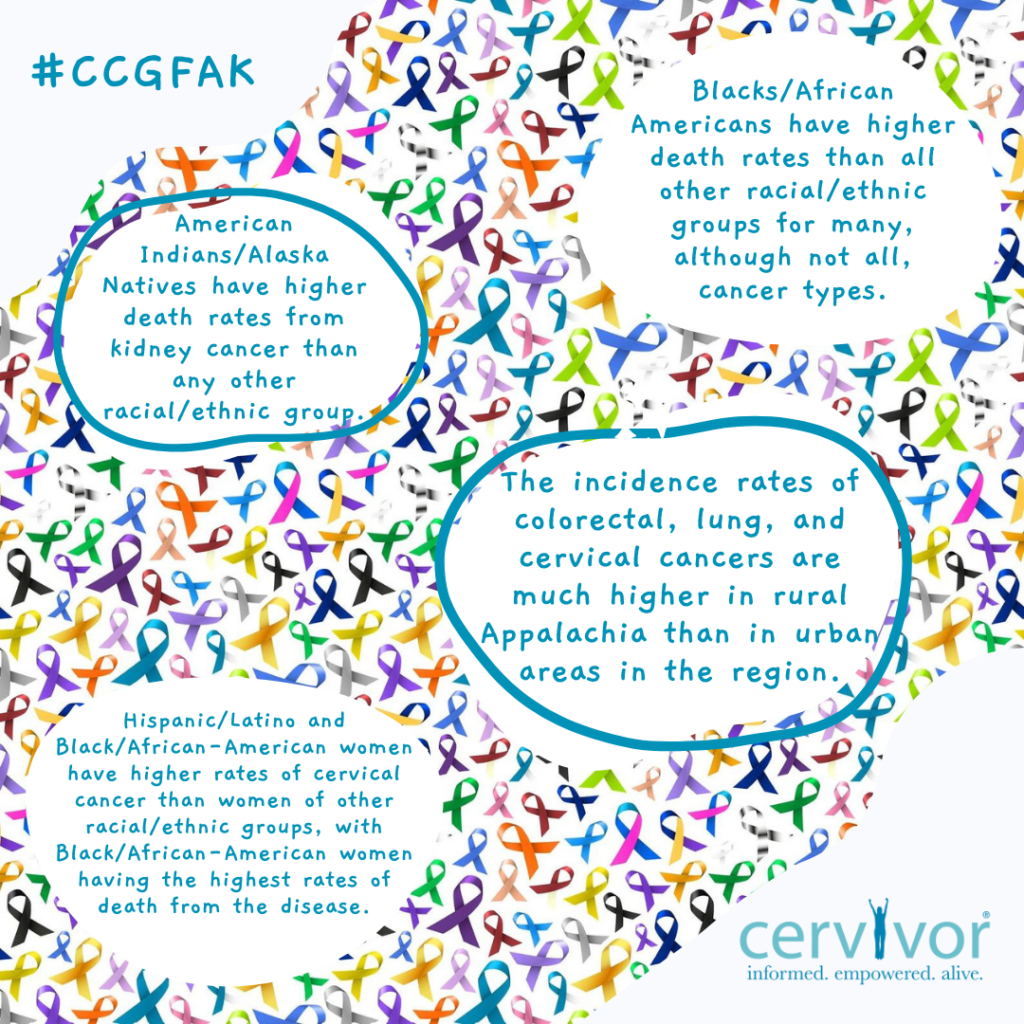
Cancer Disparities: Despite all of the improvements in technology and treatment, cancer disparities are still happening. We will continue to raise awareness on cancer disparities and share our stories to make a difference.
Global Outreach: Cancer impacts us all across the globe. We have patient advocates speaking up in Kenya, Honduras, and Saint Lucia (and many more countries) because…
Cancer remains to be the third leading cause of death after infectious and cardiovascular diseases in Kenya. Milicent and Sally use their voices to make a difference.
“So that everyone knows the importance of HPV vaccination. And to our Kenyan government to know the importance of cancer survivors – when survivors share their journey they give hope to newly diagnosed patients.” – Milicent, Kenya
“Cancer made me lose some parts of my body. Let it go fly a kite. #MakingCancerPay” – Sally, Kenya
And to change the statistics for the 56,000 women in Latin America and the Caribbean that are diagnosed with cervical cancer every year like Kadiana and Karla.
“Cancer has changed my life physically, emotionally and mentally. Although I’ve learnt to accept that I am fat and forgetful with stiff joints and many scars, cancer can go fly a kite because I am also more courageous, resilient and have a profound respect for life.” – Kadiana, Saint Lucia
“I want everyone to be able to enjoy each day, people, pets, and life. Cancer can go fly a kite and let us all live freely and healthy.” – Karla, Honduras
Survivorship: The good news is cancer deaths have declined dramatically but survivorship and quality of life matters. The number of cancer survivors is expected to increase by 31%, to 20.3 million, by 2026 and it is expected that 2 out of 3 Americans diagnosed with cancer will live at least 5 years after diagnosis.
Clinical Trials: Educating others about clinical trials because only 5% of adults with cancer will participate in them. Clinical trials are a great way to help others and gain access to the latest treatment options before they are available to everyone else.
Prevention Tips: We know prevention and early detection saves lives but what can we do to help prevent cancer? We gathered a list of helpful tips to share!

To Honor: We took the time to remember and honor those in our community who are no longer able to tell their stories. We carry their memories with us every day and find new ways to honor them.
Bernie Brennan flew a kite a kite in Ireland for her daughter, Laura Brennan. Laura was a Cervivor Ambassador and sadly, died from cervical cancer in 2019. While she was alive, she served as a Cervivor Ambassador and advocated for HPV vaccination and cancer prevention. During her short time with us, Laura made a massive impact to increase HPV vaccinations. We thank the Brennan family for sharing this day to honor Laura.

Thank You
A huge thank you to Rubius Therapeutics for sponsoring our Cancer Can Go Fly a Kite event and for continuing to find new and improved treatments for HPV-related cancers. To find out more, visit their website: https://rubiustrials.com/hpv-cancers/.




