We have to talk about the other side of cervical cancer. The side of loss.
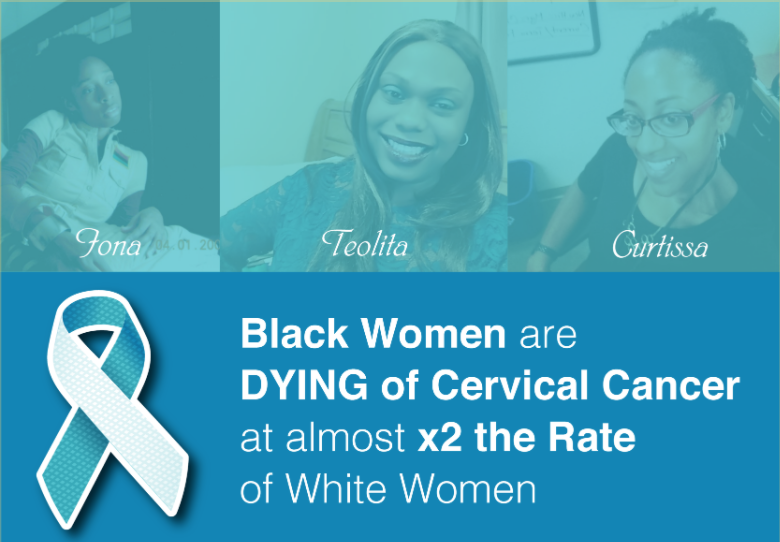
These are just some from our community and beyond who have died from cervical cancer. Their stories not only matter, they need to be perpetually in motion. Everything we do as an organization includes their footprint — their hope for a different future.

We met some of them from attending Cervivor Schools together, and others we got to know in virtual settings like Creating Connections and through our Facebook group I’m A Cervivor!. Some people come into our community seeking support from others who truly understand the burden of cervical cancer and others decide that patient advocacy is their calling.
It is truly our stories that connect us. These stories that we read and reread, often finding an intersection with so many of them. These stories continue to fuel us, inspire us and give us our wings, as Holly Lawson would often say.
Many of these women never hesitated in offering support to others. Each brought their own strength, humor and honesty to so many inside and outside of Cervivor. Like Grace, who found Cervivor in 2020 and was a huge presence within our virtual community. Many were also dedicated advocates who were shame resilient and knew they wanted to transform the narrative of cervical cancer.
Nothing about having or living with cervical cancer is easy and dying from it brings a great sadness that ripples through our community, leaving us devastated yet profoundly grateful for the experiences we shared. Together we find comfort and the strength to move forward with purpose.
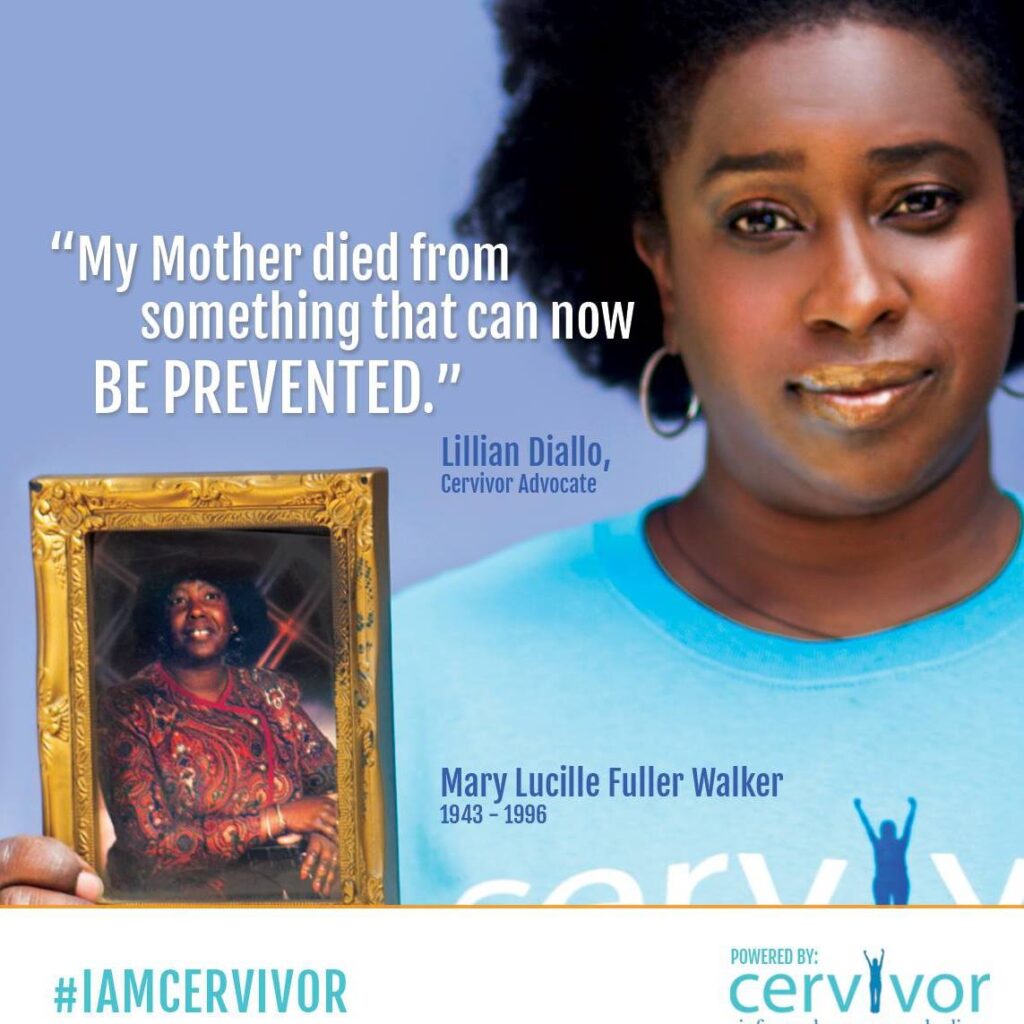
The fact that our sisters, mothers, daughters, partners and friends continue to die from cervical cancer means our work and support is crucial. We will always remember those who sought connection, an understanding of their disease or the willingness to shine a light on cervical cancer.
Cervical cancer is the fourth most common cancer in women. In 2018, there were approximately 570,000 new cases of cervical cancer diagnosed globally and about 311,000 died from the disease. Cervivor wants to change these statistics.
By honoring these and so many other women, we make a promise to carry on their legacies in the work we do every day. Together. We will not stop.
Jeanette Acosta… We will not stop.
Grace Chantiam Bracci… We will not stop.
Laura Brennan… We will not stop.
Curtissa Clay… We will not stop.
Amanda Filkins… We will not stop.
Kristen Forbes… We will not stop.
Debbie Jane Forsyth… We will not stop.
Rebekah Elizabeth Fowler Griffin… We will not stop.
Dawn Fraga-Mejia… We will not stop.
Lisa Riebersal Moore… We will not stop.
Alissa Gores… We will not stop.
Elizabeth (Lizzi) Marie Haas… We will not stop.
Princess Ruth Joanna Howard… We will not stop.
Dr. Tessa Maria Klein… We will not stop.
Holly Latrelle Lawson… We will not stop.
Christine Lerch… We will not stop.
Heather Lyn Martin… We will not stop.
Angela Mckibben… We will not stop.
Catherine “Cat” Odderstol… We will not stop.
Iona Pierre… We will not stop.
Kelly Pozzoli… We will not stop.
Brittaini Qadri… We will not stop.
Nanette Quitanilla… We will not stop.
Teolita Rickenbacker… We will not stop.
Jillian Scalfani… We will not stop.
Erica Frazier Stum… We will not stop.
Brittany Wagner… We will not stop.
Mary Lucille Fuller Walker… We will not stop.
Becky Wallace… We will not stop.
Carneese J. Williams-Ackles… We will not stop.
If you would like to honor a loved one who has passed from cervical cancer, please fill out this form.