I always thought that I’ve done very well in building up resilience, taking care of my physical and mental health, since that is basically what I do for a living. I am a Psychotherapist and am specialized in Cognitive Behavioral Therapy (CBT). I love the CBT approach in working with clients since it is a here-and-now approach, is time-limited, and is structured. I offer individualized treatment plans for each client that outline clear behavioral goals, as well as take an active role in coaching my clients by directing their therapy and assigning homework.
After undergoing a biopsy, my OB/GYN told me on my daughter’s 2nd birthday, “Unfortunately, it’s cancer”. I just sat there, repeatedly saying, “No, that can’t be true!”. I completely went into freeze response. It was like an out-of-body experience, while I was standing on the Edge of the Abyss, all around me was complete darkness. As I was shaking and crying, all I could continuously say was, “No, that can’t be true!”.
(The definition of Fight, Flight, Freeze or Fawn is the body’s natural physiological reaction to stressful events. It is activated by the perception of threat, quickly igniting the sympathetic nervous system and releasing hormones to reach the underlying goal of springing into fight, flight, freeze or fawn to decrease, end, or evade danger and to return to a state of calm and control.)
My OB/GYN’s office scheduled my first CT scan for three hours later and as my husband, who was thankfully with me at the appointment, brought me outside the office, I started throwing up while I talked to my sister on the phone telling her, “I have cervical cancer”.
At this point, I knew nothing about “my cancer”. Had it spread? Am I going to die? What stage am I? Will I see my girls graduate high school? Is it treatable? What is the chance that my cancer can be cured? What other tests and procedures do I need? How can I deal with that? I’m not the type of person that will be able to handle something like this.
The day after my diagnosis, there I was, sitting with all those thoughts, feelings, and emotions, not knowing what to do. I knew nothing anymore; I wasn’t even able to think. On this beautiful summer day, everything seemed to disappear into this deep fog surrounding me.
I, the psychotherapist, who always comes up with great treatment plans for all kinds of mental health problems my clients are dealing with, but who is now unable to even stop my own thoughts and worries. Wow, great job. I was disappointed in myself. I was disappointed in what my body had done to me by developing this cancer. And on top of that, I wasn’t even able to drag myself into a more positive state of mind. Hell, I could not even think one, clear thought.
So, when I wanted to cry, I cried. When I wanted to scream, I screamed. When I wanted to sleep, I slept. When I wanted to talk, I talked. And I went on walks, a lot of quiet, long walks. At one point, I went on Google and gathered information about cervical cancer. I reminded myself about one of the things I tell my clients, “Information is on the other side of fear”.
Then I realized that what is happening is grief. I’m grieving my cervical cancer diagnosis. I’m right in the middle of it and my psyche is doing what it’s supposed to do all on its own.
We usually reserve the word, grief, for loss, secondary to death. Well, that’s just one form of grief. Grief is an adjustment to loss. When we get our cancer diagnosis, that is loss. Loss of potential quality of life, loss of certain physical functionality. It may even be the loss of time. At some point, everyone WILL go into grief. However, not everyone will go through the stages in a prescribed order, there is no linear and predictable pattern, and we often switch back and forth between the stages.
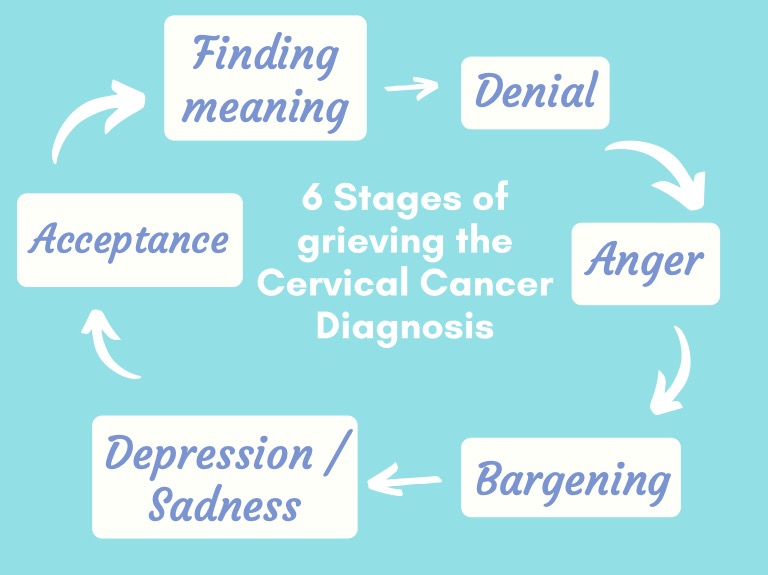
The classical, six stages of grief are simply tools to help us frame and identify what we may feel during our cervical cancer journey:
Denial: Feelings of avoidance, shock, fear, confusion. Believe that the diagnosis is somehow wrong and holding on to a different reality.
“I feel fine.” – “No, this can’t be happening to me.”
Anger: Feelings of frustration, anger, anxiety. Faced with the new reality, looking for someone/something else to fault, to leash out.
“Why me?” – “It’s not fair.” – “How can this happen to me.”
Bargaining: Struggling to find meaning. Seeking to get out of facing the new reality by promising something to change or to do differently or seeking for help through a higher power.
“I’ll do/give anything for a good outcome/a few more years.”
Depression / Sadness: Feelings of being overwhelmed, helpless, hopeless. Settling into sadness and unable to move forward.
“Live will never be the same…” – “What’s the point of going on?”
Acceptance: Feeling of exploring different options, a new plan in place, moving on. Embracing the new reality and finality of what has happened.
“I’m going to be ok.” – “I can fight it.” – “I may as well prepare for it.”
The more we give grief space to run its course, the more likely we are to have a better outcome. Sometimes we feel guilty for taking too long to grieve. NO, WE DON’T TAKE TOO LONG! Emotions work their way through us, don’t fight them, don’t rush them.
Years ago, I went to a lecture about grief and the professor added “Finding meaning/Purpose” as the last stage of grief in the circle and that stuck with me. Now, I always add that stage for my clients because I have experienced it myself.
Finding meaning/Purpose:
- Help other people with the same diagnosis by sharing your story
- Write a book
- Pull back from work/toxic people
- Join an organization
- Smell/water flowers
- Take a walk every day
- See the beauty of life
For me personally, finding meaning/purpose just started in November 2021 (yup, not too long ago), when I decided to participate in one of Cervivor’s Creating Connections virtual meetups. I’ve always been pretty private about my cancer diagnosis. I was terrified about this cancer, I just wanted it to go away, I did not want to share anything with anyone other than my closest family.
At this first meetup, I literally just listened to the other participants and there was so much hope, so much encouragement, and so many awesome ideas being shared for the upcoming Cervical Cancer Awareness Month (CCAM) in January, that I decided to participate in a second meetup. There, I started to introduce myself, shared a little bit of my story, and thought about ways to integrate some mental health ideas into CCAM.
Since then, I participated in Cervivor’s CCAM virtual activities and even spoke about self-care and mental health at the Cervivor Summit 2022. And today, here I am, continuing to find my meaning/ purpose.
“Cancer cannot cripple love, it cannot shatter hope, it cannot conquer the spirt.” ~Author Unknown

Jessica Martin was born in Germany and holds a M.Sc. in Psychology. She moved to the USA in 2018 and was diagnosed with cervical adenocarcinoma 1B2 shortly after her move. Jessica is passionate about the mental health aspect for healing.
If your cancer treatment team included an oncology social worker, could they have helped you during that moment? Would education about natural grief responses be helpful in-the-moment? Or are we too numb in the moment to hear / understand psychoeducation?
Hello Jessica,
Thank uou so much for sharing some of your story here.
I actually joined this group years ago when I first was diagnosed yet never really got involved, just a quick look through the emails once in a while.
I also was diagnosed with Cervical Adenocarcinoma stage 1b2, that was back in the fall of 2011.
I actually was misdiagnosed as I was told I only had some precancerous legions and would need a hysterectomy.
My instincts, my gut, & my nursing knowledge told me otherwise, but I was made to feel as though I was a hypochondriac every time I raised an issue that perhaps it could be something more, what did I know?
I certainly am not the poster child for nurses of America but I could read my own lab results which said directly on it “invasion could not be ruled out”, but why should I have let that bother me, right?
Anyway, long story short due to the error I not only had the surgery but had to have external & internal radiation as well as chemotherapy.
I remember all the different woman I met in waiting rooms for this or that and they all seemed to have breast cancer, I never met one person who had the same diagnosis I did and this made me feel very alone & isolated. I remember asking if their were any groups of woman with this type of cancer meeting anywhere yet the cancer center knew of none. So I just went on along my journey without a person I could reach out to to discuss my concerns, questions, fears.
This past fall marked 10 years for me since I was diagnosed and I am great full for my health however I recall so many things I wanted to do to bring awareness to this disease, I had so much anger regarding many issues I went through and was determined to make a difference to help others, yet I never did.
My health is ok as I said I am greatful however I changed after I went through my experience with cervical cancer.
You spoke of grief, I still grieve the person, the woman I once use to be. I have accepted myself & the way things are and I think I’ve let go of a lot of the anger but while writing this now I’m realizing just how quickly all of the emotions can come right on back from wherever deep down inside I have tried to hide them.
Anyway, enough of me already.
I would be so grateful to uou to hear more about your story and what you went through. I hope uou are doing ok now, and have come through whatever treatment protocol they developed for you with much success.
God Bless,
Christine Mack
[email protected]
I have found it odd that my response just went to acceptance and do what I had to do. No grief or anger or bargaining. Could have rung a bell for chemo yesterday, didn’t find it meaningful. I find myself completely detached emotionally from the situation and when I end treatment soon, I am on to better things.
What’s THAT all about!? I wonder if it’s my diagnosis not being particularly dire compared to someone with real stage 2-4 challenges. Or if I am heading for a total breakdown when I least expect. Emotional dissociation isn’t unusual for me.