By Kyle Minnis, Cervivor Communications Assistant
Peer-led advocacy isn’t just powerful—it’s transformative. According to the National Library of Medicine, programs like Cervivor School—Cervivor’s highly regarded ambassador training program—have quadrupled cervical cancer screening rates in some underserved communities.
Peer and patient advocates provide support to those undergoing treatment, help reduce the stigma of cervical cancer and other conditions, and educate people about prevention and early detection. Perhaps most importantly, they improve survival outcomes. Their work ensures patients are seen and heard while also making the healthcare system more effective and equitable.
To mark National Patient Advocacy Day (August 19), we’re diving into what patient advocacy is, its various forms, and how it has shaped cancer care since the 1950s, when patients and families first began speaking out.
We’ll also celebrate the impact of advocates in our Cervivor community—from everyday actions to global initiatives—and share ways you can get involved in this life-saving work.

What Is Patient Advocacy in Cancer Care?
First, let’s define what patient advocates do.
Clinical patient advocates—also called navigators or representatives—help patients understand their diagnosis and options, schedule and keep appointments, navigate insurance, secure resources like transportation or childcare, and coordinate care among multiple providers. Their core principle is to listen to, inform, and empower patients to actively participate in their care.
“A patient navigator is the person who makes the healthcare system accessible,” explains certified navigator Nancy Peña, OPN-CG, CMI, BA, who spent more than a decade in gynecologic oncology clinics at Dana-Farber Cancer Institute (DFCI) and Brigham and Women’s Hospital (BWH). “We keep the care plan on track, the information clear, and the patient’s goals at the center. The navigator is the bridge between the patient and the medical team.”

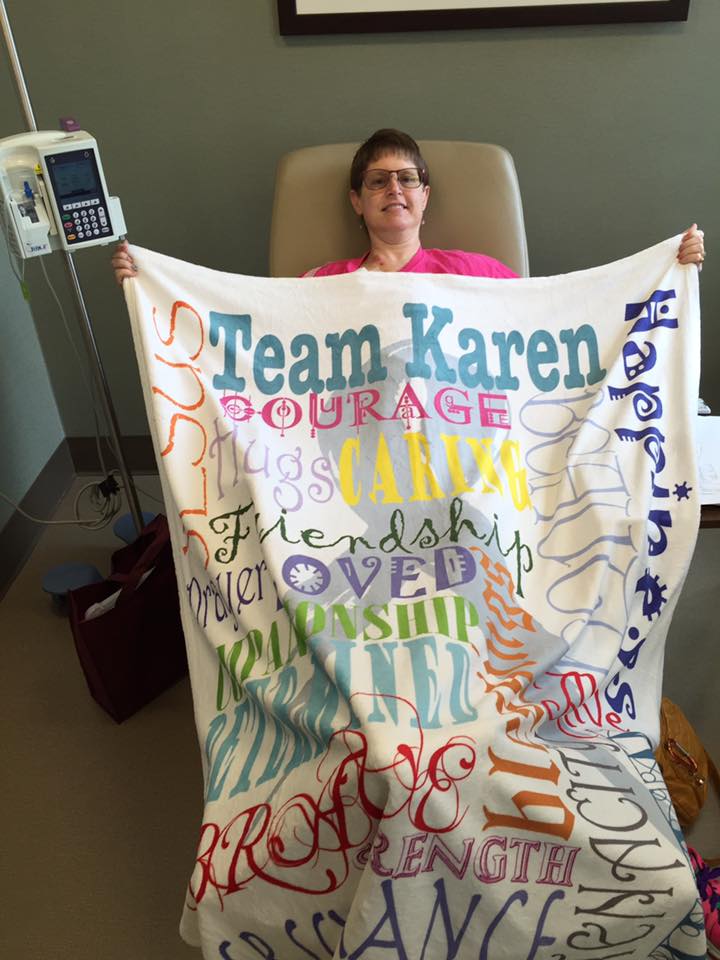
Meanwhile, nonclinical advocates—often survivors themselves—focus on building trust, hope, and community connection. Cervivor community member Sharica Lewis, diagnosed with Stage IB2 cervical cancer at age 35 in 2015, shares her journey publicly on Facebook to inspire others.
“Advocacy gives me the opportunity to share my story and support someone who may be struggling to ask questions or speak up,” says Sharica, who graduated from Cervivor School Minneapolis last year and launched her advocacy work by organizing a local cervical cancer awareness walk in her Texas town.
Nancy, who is also the Founder and Director of Navegación de Pacientes Internacional (NPI)—which trains clinical and nonclinical patient advocates in Spanish across the U.S. and Latin America—says the two types of advocates complement each other. Their goal: helping patients navigate the healthcare system while addressing emotional, cultural, and financial barriers to ensure high-quality care for all.
How Patient Advocacy Improves Cervical Cancer Outcomes
Recent studies and national summits have shown that peer and patient advocates significantly increase cervical cancer awareness and prevention—as noted above, sometimes increasing screening rates by up to four times.
Why does this matter? Regular cervical cancer screenings have cut incidence and mortality by more than 50% over the past several decades, largely thanks to the Pap test, according to the American Cancer Society Cancer Action Network (ACSCAN). Yet diagnoses in women aged 30 to 44 rose about 1.7% annually from 2012 to 2019, likely due to lower screening rates and gaps in prevention outreach, reports the American Cancer Society (ACS). These numbers make one thing clear: Screening saves lives—and advocates are essential to keeping it top of mind.
Effective hospital patient navigation programs can also have a measurable impact. “At DFCI/BWH, we reduced the no-show rate [for appointments] from 49% to 29% in the first five years,” says Nancy. “This success was possible through staff collaboration, consistent patient education, and multi-lingual resources that ensure every woman knows her next step.”
How Patient Advocacy Helps Close Healthcare Disparities
Here are some sobering facts: In the U.S., Black women are twice as likely—and women living in poverty four times as likely—to die from cervical cancer compared to white women. American Indian and Alaska Native women face two to three times higher mortality, while rural women are more likely to be diagnosed late and die from the disease.
These disparities underscore the vital role patient advocates play in closing gaps in care and ensuring prevention and treatment reach those who need it most.
Patient advocacy organizations like Cervivor and Nancy’s multilingual, multinational NPI respond to these challenges by offering localized, culturally competent support, adapted education, and strong policy engagement. They earn trust by meeting women where they are and truly listening to their needs—something clinics alone can’t always do.

Both clinical and nonclinical are irreplaceable for designing inclusive cancer care. As Nancy explains: “Native-language navigation improves informed consent, adherence, and satisfaction; reduces errors and no-shows; and honors dignity. When a woman can understand her options and feel supported, outcomes improve—and families and communities feel the difference.”
Advocacy in Action: Sharing Cervical Cancer Survivor Stories
Honduran native Karla Chavez—a Cervivor Ambassador and co-leader of the Cervivor Español community—was diagnosed with Stage II cervical cancer at age 34 in 2017. After completing treatment, she says Cervivor was a “lifeline.”
“Attending Cervivor School in 2019 gave me the knowledge, confidence, and community I needed to take my advocacy to another level,” says Karla. “They provided training, resources, and a network of incredible survivors who inspire me daily.”
Since then, the award-winning advocate has participated in outreach through the 2024 Communities of Color Advocacy Training Retreat and delivered remarks during last year’s Cervical Cancer Elimination Day of Action (November 17) at a World Health Organization–hosted webinar.

Similarly, Cervivor Ambassador Emily Hoffman—diagnosed with Stage II cervical cancer and treated in 2013—has made advocacy a central part of her life. Her “airplane advocacy”—simple, one-on-one conversations, often sparked by the HPV button she wears—can be just as impactful as speaking at larger events, like her home state’s Iowa Vaccination Summit, where she presented last September.
Emily also champions cancer registries, which are essential for improving patient outcomes and securing public health funding. In 2020, she became a certified cancer registrar, sharing, “Knowing my work could impact cancer advocacy, policy, and research—that’s the fulfillment I was looking for.”

How to Get Involved in Patient Advocacy
Patient advocacy is more important than ever. Public health initiatives—including the CDC’s National Program of Cancer Registries (NPCR), which has helped reduce U.S. cancer death rates by 34% since 1991—face increasing threats.
If getting into patient or survivor advocacy feels overwhelming, take inspiration and advice from these Cervivor community members.
“Start small and start from the heart,” says Karla. “At first, I didn’t know how to share my story—I was still processing everything I had gone through. What motivated me was the feeling of isolation. I didn’t know anyone else who had experienced what I had. I wanted to talk to someone and not feel alone.”
Sharica takes a similar approach: “My tag line is, ‘Let’s start the conversation!’” she says. “Cervivor has empowered me by giving me a community that understands me and everything that I’ve been through. Any opportunity I get to advocate, I’m grateful for it. I get excited when I post on social media and a parent comments that they had their child vaccinated.”

Ready to get involved? Here’s how:
- Join a support group or peer network like Cervivor, which hosts monthly virtual meetups and other opportunities to connect with fellow survivors.
- Attend advocacy trainings through programs like Cervivor School. (Applications sign up Friday, August 22, so sign up now for next month’s Kansas City training!)
- Share your Cervivor Story—on social media, in your community, or at local events.
- Volunteer for patient- or survivor-led initiatives.
- Donate to organizations like Cervivor that empower patient advocates. (Our Tell 20, Give 20 fundraising campaign is ongoing—learn how to join and help save lives!)
- Contact policymakers and lend your voice to legislative efforts that expand access to prevention, treatment, and care.
As patient navigation and advocacy continue to grow—with expanded training, certification programs, multilingual initiatives, and recognition by hospitals and public agencies—there’s hope that equitable care will become the norm, not the exception.
Nancy sums up the work well: “Navigation is a practical expression of equity.”
Together—by sharing stories, showing up for each other, and pushing for change—patient advocates are leading the way toward ending cervical cancer and building a future defined by equity, support, and survivor strength.
Honor National Patient Advocacy Day by sharing this post and joining the mission to end cervical cancer!
About the Author

Kyle Minnis is a senior studying Strategic Communications at the University of Kansas. He is currently serving as Cervivor’s Communications Assistant.