What’s filled with practical tips, inspiring stories, and essential information for newly diagnosed cervical cancer patients—and features the Cervivor community throughout?
Drum roll, please…
It’s the brand-new Patient Resource magazine, published in partnership with Cervivor, Inc. and supported by Pfizer.
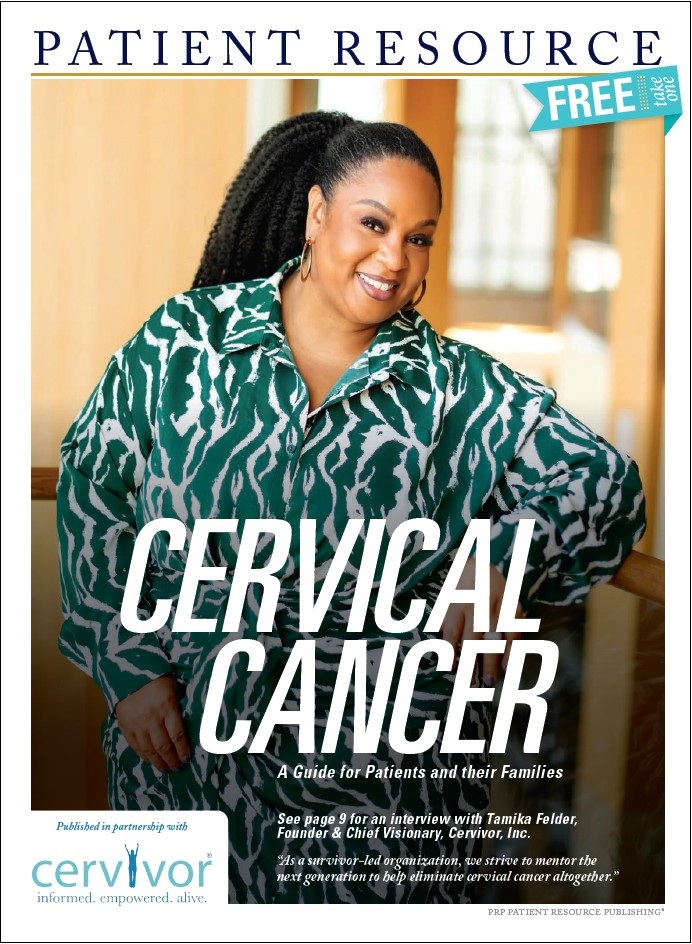
From the cover story spotlighting Cervivor Founder and Chief Visionary Tamika Felder to easy-to-understand infographics; useful charts on cancer staging, treatment side effects, and patient resources; and thoughtful guidance on emotional wellness, survivorship, caregiver support, and more—this edition is a must-read for anyone navigating the cervical cancer journey, as well as for loved ones walking alongside them.
Available for free in doctor’s offices, cancer centers, and clinics nationwide, the guide also features:
- A 20th-anniversary tribute to Cervivor
- A personal story from Cervivor community member Lisa Lakey
- Tips and encouragement from Ambassadors Anna Ogo and Karen North
Can’t wait to read it? You can also download the full digital edition and read it cover to cover right now.
This collaboration underscores how vital partnerships are in expanding our reach and delivering life-saving education and support. Huge thanks to Patient Resource and their top-notch team for helping bring this vision to life!
How You Can Support Cervivor’s Mission
- Order Your Guide: Get your free print copy of the Patient Resource cervical cancer guide to arm yourself and your loved ones with knowledge.
- Share Your Story: Your voice has power. Connect with us and share your experience to inspire and educate others.
- Support Our Mission: Every contribution helps us continue our vital work in awareness, education, and support.
- Stay Connected: Follow us on social media, sign up for our newsletter, or subscribe to our podcast to stay informed and engaged.
United in purpose, we can make cervical cancer a thing of the past, empowering a future where everyone with a cervix can live free from this disease.
Reprinted with permission from Patient Resource LLC. © Patient Resource LLC 2025
