By Kyle Minnis, Cervivor Communications Assistant
Each year, Hispanic Heritage Month (September 15 to October 15) honors the contributions and resilience of the more than 65 million Hispanic Americans who shape our nation’s culture, economy, and communities. It’s also an important opportunity to highlight persistent health disparities—particularly in cervical cancer prevention and treatment, which disproportionately affects Latina women.
Latinas are 43% more likely to be diagnosed with cervical cancer than non-Hispanic white women, and their risk of dying from it is 25 to 50% higher, according to the American Cancer Society (ACS). They receive significantly fewer Pap tests and are less likely to follow up on abnormal results, reports the Centers for Disease Control and Prevention (CDC). Barriers to care include stigma and silence around “below-the-belt” cancers, language differences, insurance gaps, transportation challenges, and inflexible work schedules, all of which delay diagnosis and limit access to lifesaving interventions.
Patient navigators like Nancy Peña—Founder and Director of Navegación de Pacientes Internacional (NPI), which trains Spanish-speaking clinical advocates across the U.S. and Latin America—champion bilingual education and culturally competent care, explaining, “Native-language navigation improves informed consent, adherence, and satisfaction; reduces errors and no-shows; and honors dignity.”

HPV vaccine uptake among Hispanic youth and young adults also remains low. While 63% of U.S. adolescents ages 13 to 17 are up to date on the full series, Hispanic adults ages 18 to 26 lag behind: According to the latest National Health Interview Survey, only 36% had received at least one dose, and just 21.5% had completed the full series—far below the national goal of 80% two-dose completion by age 15.
As Cervivor has reported, in many traditional households—Hispanic or otherwise—the vaccine is still seen to promote promiscuity. “It’s so important to speak openly with our children about cervical cancer and the HPV vaccine,” says cervical cancer survivor Maritza Manjarrez, a Cervivor Español member who was raised in a Mexican family. “Vaccinating our youth doesn’t mean we’re giving them permission to have sex—it means we’re protecting them from a cancer that can develop later in life.”
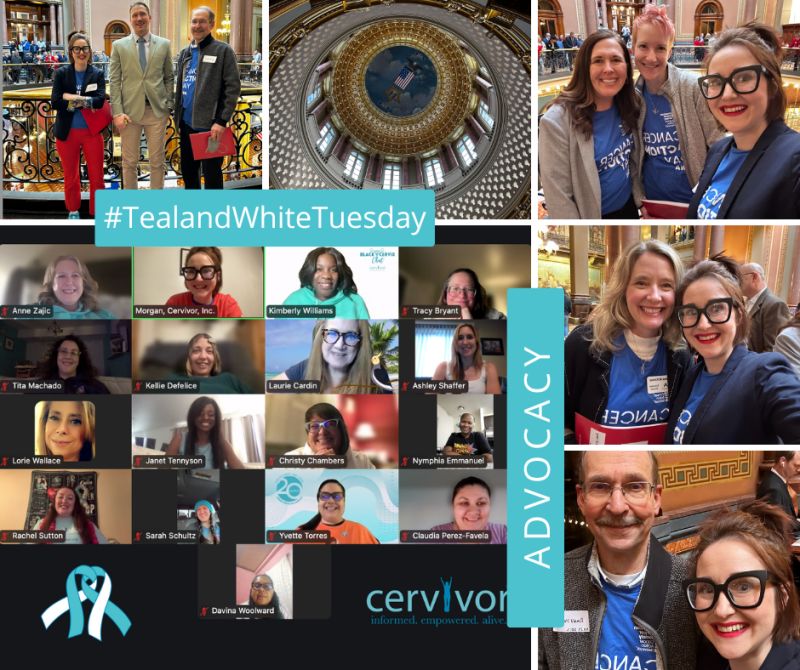
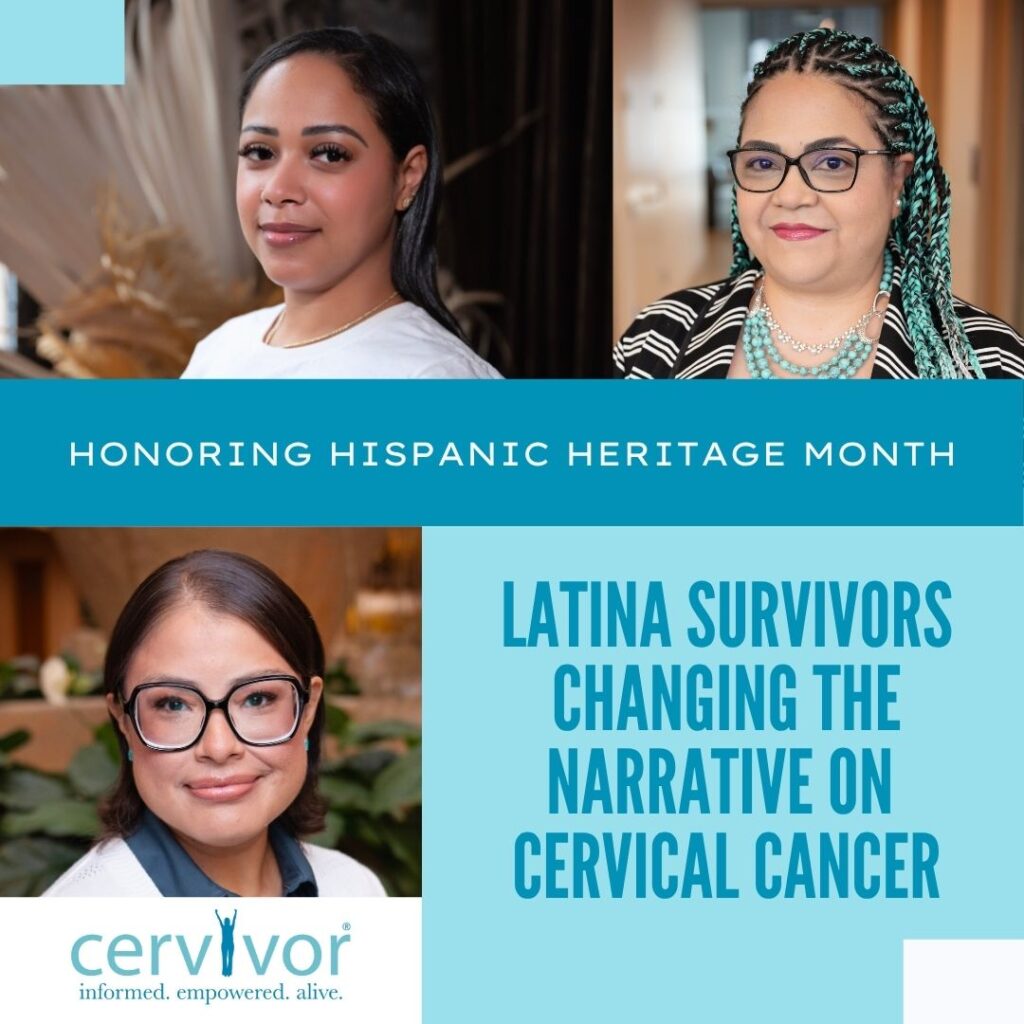
Cervivor’s mission is to help eliminate cervical cancer while also lifting survivors from isolation, providing community and education, and empowering those affected to become advocates. This Hispanic Heritage Month, we celebrate our Latina community members—including Maritza, Dulcely Tavarez, Yvette Torres, and many more—by amplifying their stories and strength. Their voices demonstrate what it means to live beyond cervical cancer while advocating for health equity and compassion.
Maritza Manjarrez: Breaking the Silence

“My cervical cancer journey has been especially difficult as a Latina. The stigma surrounding HPV and cervical cancer in our community has played a huge role in that,” says Maritza, who was diagnosed with metastatic squamous cell carcinoma at age 34. “Growing up Mexican meant you didn’t talk openly about topics like this. Keeping what was considered ‘private information’ to myself made it very hard to find help, support groups, or even basic information.”
That silence meant it took Maritza years to find Cervivor and feel comfortable sharing her story. “When asked what type of cancer I had, I felt a sense of shame and embarrassment to answer cervical cancer,” she recalls. “I believe this stigma plays a big role in the statistics. It makes me sad and worried, because if we don’t increase advocacy, these numbers are not going to change. Too many of our women are dying from this preventable disease.”
Dulcely Tavarez: Shattered Dreams, Renewed Fire

Dulcely describes being in her early twenties, putting her own health last while caring for others, a struggle familiar to many Latinas. In April 2015, she finally saw a doctor about her irregular menstrual cycles, but was bounced between providers before receiving a cervical cancer diagnosis. “‘Later’ almost cost me everything. By the time I was diagnosed, the treatment I needed was life-saving but meant I could never carry a child.”
Dulcely’s family surrounded her with care and love, but it sometimes intensified her grief and isolation. “In our community, family and children are seen as such a natural part of life that it’s hard to explain the emptiness when that dream is taken away. Even when they were trying to comfort me, sometimes I felt alone in those emotions.”
She found healing in Cervivor. “When I looked for stories that reflected my own—young, Latina, facing cancer and fertility loss—I couldn’t find them. And that loneliness can be crushing. We need to see ourselves in these campaigns, in our own language, in ways that reflect our values and struggles. Representation is not just about visibility—it’s about saving lives and healing hearts.”
Thanks to her involvement with Cervivor, Dulcely became the first-ever recipient of the Cervivor Baby Gift Fund at this January’s 2025 Cervical Cancer Summit. The award supports cervical cancer survivors pursuing alternative paths to motherhood and accepts donations from $10 to $50,000.

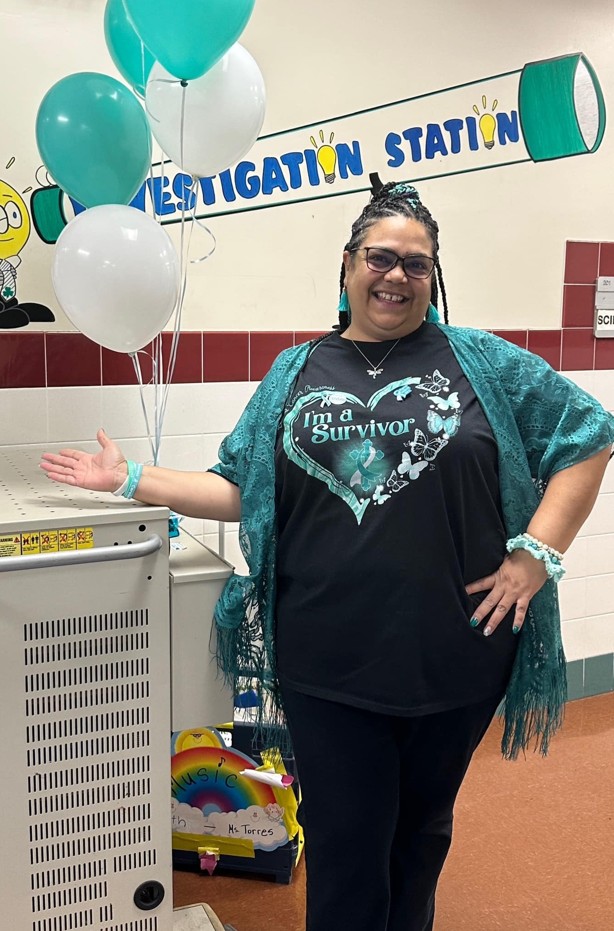
Yvette Torres: From Shame to Advocacy

Yvette’s cancer journey began with an unsympathetic, unprofessional diagnosis. “The doctor asked, ‘Why did I wait so long?’ Still in shock, I did not answer that callous question,” she recalls. At 42, she and her husband had been hoping for another child so their youngest son could have a closer-in-age sibling—but that hope ended with a biopsy, performed on her son’s 4th birthday, that confirmed cervical cancer in 2013. She remembers the OB/GYN telling her it “didn’t look good,” that it was most likely cancer, and later saying it was a “good thing I already had two children,” since treatment would likely take away her chance to have more.
This cold medical treatment reinforced how stigma and cultural silence can delay women from seeking care. Yvette shares, “I hid. I felt ashamed. I didn’t want to talk about it because that’s what I learned growing up—we didn’t talk about below-the-belt issues. My mother did teach me the importance of going to the gynecologist. However, I did not feel comfortable talking about details, differences, or changes in my body.” Her experience echoes what many Cervivor Español members describe: how misconceptions about HPV, reluctance to discuss gynecologic cancers, and language barriers all contribute to lower screening and vaccination rates.
For Yvette, community was the turning point. “I found Cervivor during COVID, when isolation made everything feel even worse.” Through Cervivor Español, she gained the confidence to speak out in Spanish, even though she hadn’t grown up fluent, and now distributes bilingual prevention materials. “Now, I celebrate and embrace my Black and Hispanic identity by advocating for these communities and helping women not feel ashamed by sharing my story,” says Yvette, a 2023 Cervivor Champion and recent top Tell 20, Give 20 fundraiser, who also mobilized her students through a school workplace drive to spread awareness.

Join the Movement to End Cervical Cancer Disparities in Hispanic Communities
Latinas make up 20% of the U.S. population, and their stories of surviving cancer, overcoming setbacks, and celebrating successes deserve to be heard—not just during Hispanic Heritage Month. Whether navigating care in a new language, confronting cultural silence around cancer, or redefining family and identity after treatment, Latina Cervivors show that community and compassion can transform what’s possible.
To help reduce cervical cancer diagnoses and improve outcomes for Hispanic individuals with a cervix, take action today by:
- Sharing your Cervivor Story to put a face on a cancer that is too often hidden or hushed.
- Supporting Cervivor’s 20th-year Tell 20, Give 20 campaign to fund culturally relevant programming and Cervivor Español support group (and sign up for next month’s event).
- Advocating for bilingual programs—like Nancy Peña’s NPI patient navigators—that help create more equitable care pathways.
- Championing advocacy groups such as the ACSí Se Puede Hispanic/Latino Advocacy Alliance, which amplify voices and expand access for Spanish-speaking communities.
- Using your voice. If you speak Spanish—whether fluently or conversationally—you can support those facing language barriers. Talk with them about the life-saving benefits of HPV vaccination, regular screenings, and timely follow-ups.
Lastly, honor the voices of Maritza, Dulcely, and Yvette—and so many others—by making this Hispanic Heritage Month a catalyst for lasting change. As Dulcely reminds us:
“Please don’t wait. Don’t push your health to the bottom of the list the way I did… To the mothers—protect your children with the HPV vaccine. It’s an act of love. To my fellow women—know your worth, use your voice, and never stop fighting for answers.”
If you found this blog post helpful, please share it with friends or family members. You may just save a life. Questions? Contact us at [email protected].
About the Author

Kyle Minnis is a senior studying Strategic Communications at the University of Kansas. He is currently serving as Cervivor’s Communications Assistant.