By Morgan Newman, MSW, Community Engagement Liaison
As the Community Engagement Liaison for Cervivor, Inc., I’ve had the privilege of supporting many individuals through their cervical cancer journeys. While treatment and physical recovery often take center stage, it’s crucial to recognize the profound mental, emotional, and psychological impact of cervical cancer, which can be overwhelming, isolating, and frightening.

At Cervivor—founded 20 years ago to support those affected by the disease—we don’t shy away from facing these challenges head-on. Many in our community say that the been-there-done-that understanding and solidarity they find here play a vital role in their healing.
Janice Le-Nguyen, a Cervivor celebrating four years of being NED (no evidence of disease) after Stage 1A2 cervical cancer, shares: “I am appreciative of finding the Cervivor community and finding pathways to not feel ashamed and that I can freely discuss HPV, the cervix, and all the ‘fun’ I went through.”
I felt the same way after surviving Stage III at 24. Getting involved with Cervivor and advocating for fellow survivors helped me reclaim my voice and purpose.
But the cervical cancer journey is complex. Emotional highs and lows are part of the experience. Here are some of the most frequent mental health concerns our community members face—and why it’s so important we talk about them openly, without judgment or fear.
Survivor’s Guilt
Feeling grateful to be alive while struggling with the aftermath of treatment can bring on guilt and self-doubt, especially when others faced tougher outcomes or didn’t survive. On average, about 10 women from our immediate Cervivor community die each year—and it never gets easier to say goodbye.
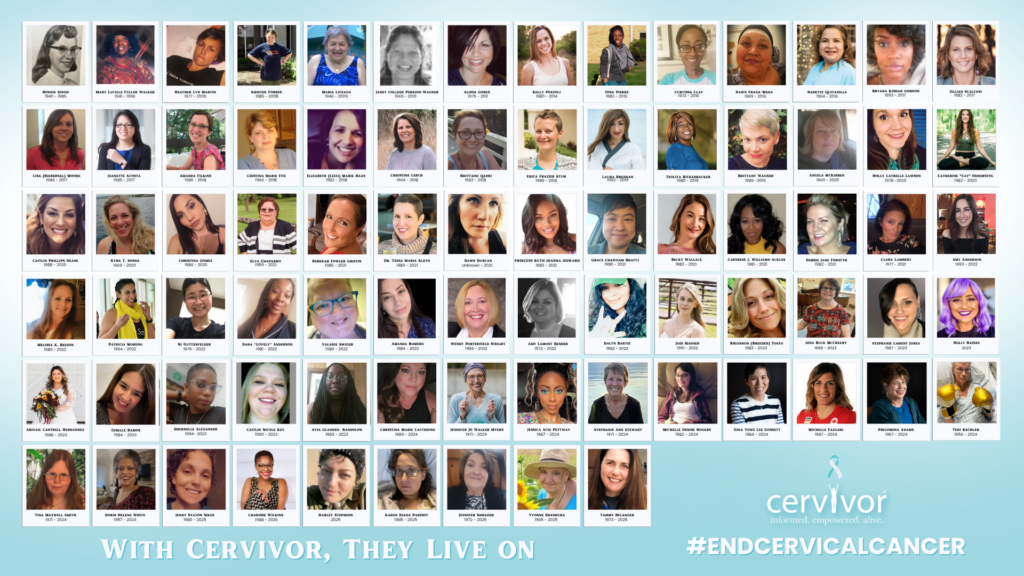
These losses weigh heavily, but they keep us grounded in our mission to eradicate the disease. Rather than staying stuck in cycles of guilt, many of us find healing through action.
That’s been true for Janice. “Through Cervivor, I realized that by sharing my story, I could inspire others to get screened, ask questions, and take charge of their health,” says the quiet but fierce advocate, who started local community outreach with Cervivor a few years back.
We encourage all survivors to share their Cervivor Stories when they feel ready—each one adds powerful momentum to our mission and gives hope to others. If you’d like to share your experience, consider filling out this questionnaire and submitting a photo.
Scanxiety and Fear of Recurrence
Scanxiety—a term widely used in the cancer community—describes the intense anxiety and fear that can build up around follow-up scans and tests.

As a metastatic/recurrent survivor, I know this feeling all too well. Nine years ago, I was given just a 7–9% chance of ever being cancer-free—and yet, here I am. Still, every new ache, pain, or side effect can feel like a potential sign of recurrence.
A supportive community makes a difference. In our Cervivor Facebook group, for example, many members openly share their experiences with scanxiety and offer practical ways they’ve learned to cope. Just knowing you’re not the only one feeling this way can bring relief. And as always, consult your health provider if symptoms arise.
Body-Related and Intimacy Issues
Changes to the body can deeply affect self-esteem and relationships. Radiation side effects, like needing a cane or wheelchair, can be life-altering. Invisible disabilities like lymphedema, ostomies, and hearing loss require constant management.
Survivors in our community, including Lead Cervivor Ambassador Carol Lacey and others like Lorie Wallace, Sara Johney, Gabrielle McCord, Mary Clarkson-Grubb, Sally Kwenda, Maria Franklin, Julie Groob, Karla Chavez, and Talitha Stempin, navigate these challenges with strength and grace. Tools like lymphatic compression gear, ostomy bags, and hearing aids become part of daily life and symbols of resilience.

Body changes can also affect physical and emotional intimacy. Survivors have bravely opened up about their experiences on the Cervivor Blog, and a recent CervivorTV video, hosted by Founder and Chief Visionary Tamika Felder and featuring Dr. Christina Wilson, a board-certified women’s health nurse practitioner, dives into navigating body image and sexual health. It’s a must-watch.
Depression
The trauma of a cancer diagnosis and treatment can trigger depression—a reality that affects up to 25% of cancer patients, according to the National Cancer Institute (NCI). Yet, only a fraction receive the mental health support they need. Left unaddressed, depression can slow recovery, weaken the immune system, and negatively impact survival.

Cervivor community member Kyana Johnson, diagnosed with Stage IIIB cervical cancer at 26, has shared her mental health struggles on the blog. She found comfort in self-care practices like journaling, meditation, coloring, and listening to music. Seeing a therapist at least twice a week was especially transformative.
“It was some of the best conversations I’ve ever had,” recalled Kyana, now seven years in remission. “My therapist helped me make sense of a lot of my emotions.”
And she offers this encouragement to others: “Remember that you are worth it. You shouldn’t be ashamed to seek mental health advice when your anxiety or stress feels too heavy.”
I’m also inspired by survivors like Danielle Glick and Jessica Martin, who have become psychotherapists since their cervical cancer experience. Their journeys show how healing mental and emotional health can lead to purpose, helping others find strength during the most difficult times.


You Are Never Alone
Because cervical cancer’s link to HPV can carry stigma, many feel isolated. But within Cervivor, we work to break that silence. We notice when someone goes quiet, we reach out, and we hold space for each other—without pressure to always “be okay.”
Ultimately, connection is essential to mental health recovery. Healing requires both safety and vulnerability. By naming and normalizing our struggles, we build resilience—and a supportive community that truly sees us. As Kyana put it, joining support groups like Cervivor helped her mental well-being because “they got it.”


Our mantra is simple: You are never alone. Whether through private groups, monthly support meetups, or personal check-ins, there is always a place for you here.
Ready to build meaningful relationships and support others in their cancer journeys? Join our monthly Creating Connections virtual meetup, designed for cancer patients, survivors, and thrivers. This supportive community is a safe space to share experiences, find resources, and connect with others who understand. Register for our next virtual meetup today.
About Morgan Newman, MSW
A resilient young adult (AYA) cervical cancer survivor, social worker, and dedicated patient advocate, Morgan has transformed her experience into a powerful force for change. After overcoming metastatic and recurrent cervical cancer at 24, she became a Cervivor Ambassador in 2017 and has since led global advocacy efforts. Her leadership roles include Community Engagement Liaison at Cervivor, board member for Above and Beyond Cancer and the Iowa Cancer Consortium, and Iowa State Lead Ambassador for the American Cancer Society Cancer Action Network (ACS CAN). She also serves on the Iowa Immunizes Coalition and as a patient advocate for the NIH’s Enduring Guidelines and Extended Genotyping Panels, and the NCI’s Patient Advocacy Steering Committee and Cervical Task Force. Morgan’s work has earned her awards and recognition, solidifying her as a leading voice in the fight against cancer.