By Sara Lyle-Ingersoll, Cervivor Communications Director
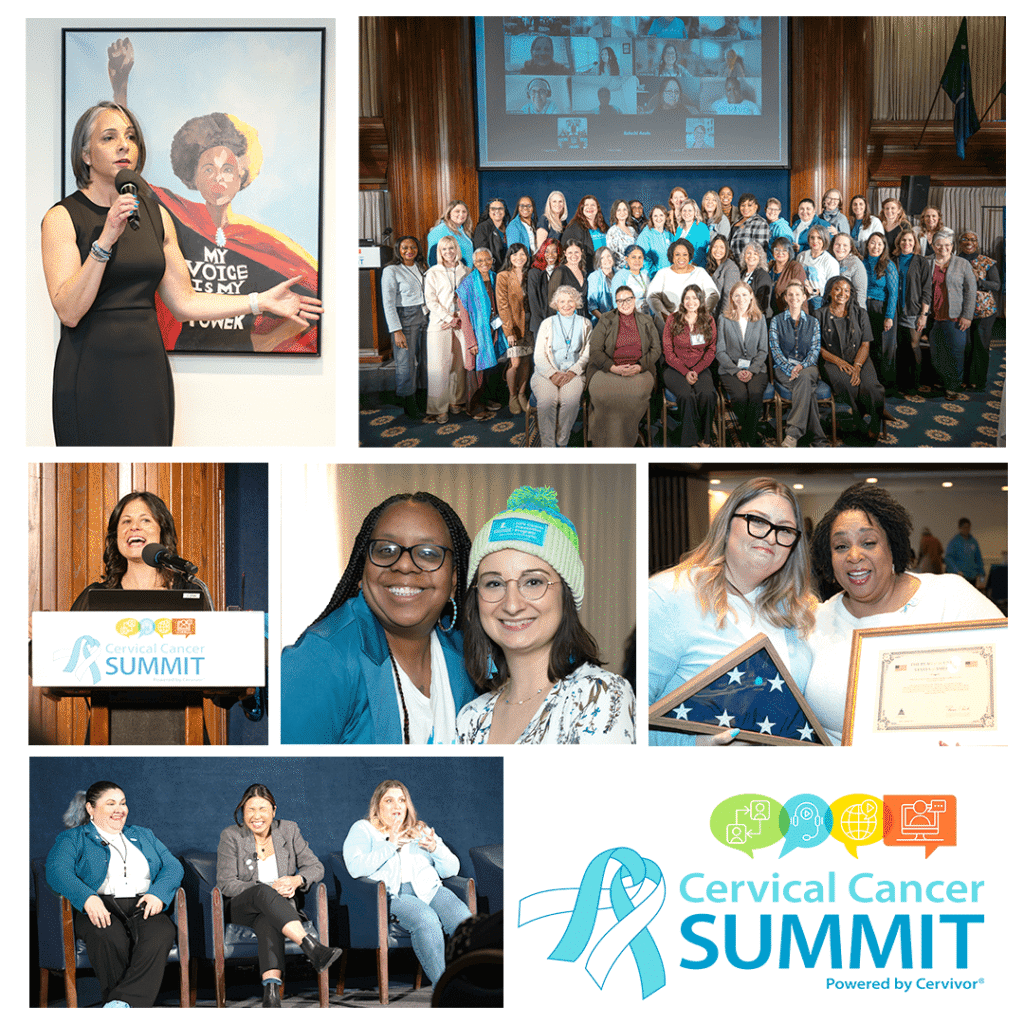
On January 23, 2026—the day after the United States formally completed its withdrawal from the World Health Organization (WHO)—survivors, clinicians, advocates, researchers, and policy leaders gathered at the historic National Press Club in Washington, D.C. for the 2026 Cervical Cancer Summit Powered by Cervivor, Inc.
The timing was not lost on anyone in the room.
For decades, the WHO has played a central role in advancing global cervical cancer elimination. As the Summit began, speakers acknowledged the moment with clarity and resolve: Global collaboration still matters, science still matters, and the work does not stop.
As Ebony Hoskins, MD, gynecologic oncologist at MedStar Washington Hospital Center, said during her morning session, “That makes it even more important that we continue to use global standards for elimination and rely on organizations like Cervivor to get the word out and engage our community navigators.”
Mission accepted, Dr. Hoskins.
At the top of the agenda, Cervivor Ambassador and Cervivor Español Co-Lead Karla Chavez welcomed both in-person and virtual attendees with a heartfelt message from Siguatepeque, Honduras. Having previously shared her lived experience as part of the WHO’s Cervical Cancer Elimination Day of Action, her perspective carried particular significance.

If you were in the room, you could feel the momentum already building toward elimination. If you weren’t, here’s what you missed.
Cervivor’s Founder: “We Make the Data Come Alive”
The packed speaker slate began with Cervivor Founder and Chief Visionary Tamika Felder’s annual State of Cervical Cancer address, reflecting on the organization’s 21 years of impact—and the work still ahead. Taking the stage to the iconic 1979 anthem “Ain’t No Stoppin’ Us Now,” she wove together her personal journey as a young cervical cancer survivor, the evolution of Cervivor from a grassroots support network into a global advocacy organization, and the power of community to transform isolation into action.

“We make the data come alive,” Tamika reminded the audience. Survivor voices give meaning to the numbers and urgency to the mission.
She challenged attendees not only to absorb the information shared throughout the Summit, but to carry it forward into their communities, healthcare systems, and policy spaces—reminding the audience that the work doesn’t end when the Summit does. “Whatever we talk about today, let’s not leave it here at the National Press Club,” she urged. “Let’s make sure everyone is talking about cervical cancer.”
An Emphasis on Evidence
Several early sessions reinforced a critical truth: We already know how to prevent cervical cancer, but access, trust, and implementation are uneven. Distinguished speakers grounded their messages in data, making the point unmistakable.
Dr. Hoskins highlighted both advances and persistent gaps, including the reality that a significant number of cervical cancer diagnoses still occur later in life and among people who were told screening was no longer necessary.

Her message was direct and evidence-based: Cervical cancer screening saves lives, innovation matters, and patients must be empowered to actively engage in their care. Her advice to patients: “Bring your questions written down. Bring a support person to be a second set of ears. Anxiety can make it hard to process information and support matters.”
That emphasis on evidence continued with Silke Schoch, MA, of the National Health Council, who showed how patient experience mapping becomes more meaningful when patients themselves help shape it. Through a striking comparison, she contrasted a “before” dry, clinically driven journey map with an “after” redesigned version that was more accessible and genuinely useful to those navigating care. Schoch also credited the launch of a tool to help organizations, academic institutions, and nonprofits equitably compensate patients for their time and expertise, saying, “Patients are all experts, and they should be compensated as experts and treated as experts.”

Next, speaking directly to the many cervical cancer patients and survivors in the audience, research expert Irene Aninye, PhD, reframed the role of lived experience in advancing change. “You are a data point—but you are more than a statistic,” she said. “When your story is paired with the numbers, people remember. That’s how progress happens.” Through interactive polling, she led the audience in discussion about the importance of prioritization and coalition-building to compel policy and systems change.

Later in the day, Michelle Fiscus, MD, FAAP, Chief Medical Officer of the Association of Immunization Managers, shed light on more solid evidence: HPV vaccination prevents cancer. Walking participants through the complex history of the HPV vaccine—with some levity along the way—she explained how what should have been a public health success story when it was introduced in 2006 instead became a breeding ground for misinformation and vaccine hesitancy. “We’ve been able to prevent cancer for 20 years,” she said, “and yet this vaccine became a firestorm almost from the moment it was introduced.”

She emphasized that strong, consistent recommendations remain essential. “The problem isn’t the science. It’s how unevenly it’s been implemented—and how easily trust can be undermined.”
From Awareness to Action
That call-to-action energy carried through every session at the century-old club. In a purposeful discussion on the impact of proclamations, Cervivor Ambassador Christy Basa Chambers captured the urgency felt across the room: “This should be called Cervical Cancer Action Month, not just Cervical Cancer Awareness Month,” she said.

A Cervivor Community Vision and Impact session demonstrated what is possible when survivors turn pain into purpose. Moderated by Cervivor Ambassador and Program Coordinator Lauren Lastauskas and featuring Cervivor Ambassadors Trish Byerly, Claudia Pérez-Favela, and Joslyn Chaiprasert-Paguio, the panel traced each speaker’s unique journey from diagnosis to advocacy—and how reclaiming one’s voice can break stigma, close equity gaps, and save lives locally, nationally, and globally.

Joslyn, who hosts the Cervivor Podcast, spoke about fertility loss, nearly losing her life during childbirth, and the realization that “you’re never really done with cancer,” adding, “That’s when I knew this had to be my path—to speak up for people who don’t always have that option.”
The session concluded with an emotional moment of recognition, when Trish presented Tamika with a flag flown in her honor—at the request of Senator Tim Kaine of Virginia—on the 74th anniversary of Henrietta Lacks’s passing, October 4, 2025.

Later, in a Community In Action session, moderated by Cervivor Ambassador Tiera Wade, panelists Adana Llanos, PhD, MPH (Columbia University), Brooke Stewart, MPH (Louisiana Cancer Prevention), and Paris Thomas, PhD, MS (Equal Hope), explored how community-rooted partnerships are critical to advancing equity. “Equity work requires sustainability,” Paris noted, reflecting her nuanced understanding of the Chicago communities she serves. “That means supporting the people doing the work so they can continue showing up without burning out.”
Brooke shared a powerful example from a recent partnership with Cervivor’s 2025 Communities of Color initiative in New Orleans, where HPV self-sampling was brought directly to a neighborhood parade and dozens of women were tested on the spot. “It was just beautiful,” she said.

Treating Patients as Stakeholders
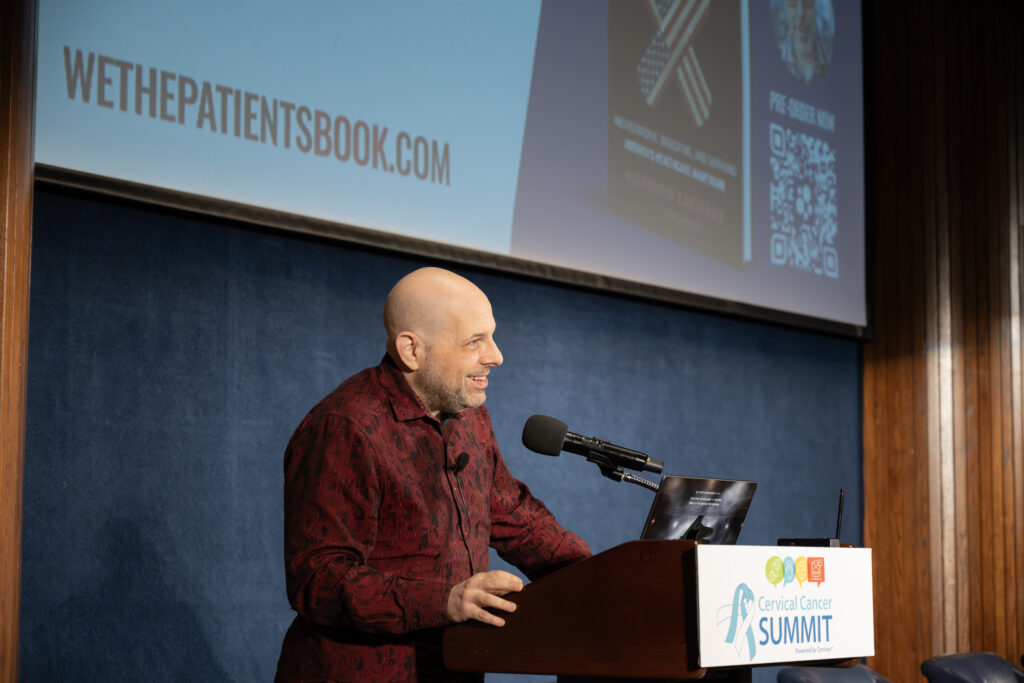
Ahead of the Summit, keynote speaker Matthew Zachary, founder of Stupid Cancer and We the Patients and longtime Cervivor ally, reflected publicly on why the gathering mattered. In a LinkedIn post, he wrote:
“Cervical cancer exposes the system in plain sight. Prevention exists. Screening exists. Treatment exists. People still die because access collapses along lines everyone pretends not to see.”
Zachary carried that clarity into his highly anticipated session, speaking candidly about survivorship, power, and the role of organized patient voices in shaping systems change. He also read publicly for the first time from the acknowledgments and foreword of his upcoming book, We the Patients: Understanding, Navigating, and Surviving America’s Healthcare Nightmares, offering a deeply personal reflection on the influences that shaped his work—including his younger self, who survived brain cancer in his early twenties, and those who did not make it.
Following, Cervivor Ambassador Kate Weissman slipped into glittery “teal heels” on stage before sharing her cervical cancer story and how it propelled her into legislative advocacy. Diagnosed at age 30, Kate detailed how an insurance denial forced her family to pay $100,000 out of pocket—an experience that later led her to become the lead plaintiff in a historic, multi-year class action lawsuit and policy changes that closed loopholes insurers used to deny care.
“You don’t have to be a policy expert to advocate,” she encouraged fellow survivors in the audience while demystifying lobbying. “You just need to show up, tell the truth about your experience, and connect it to why change is needed. Lawmakers remember stories. They remember faces.”

Kate also announced a new Cervivor Survivor Policy and Advocacy Working Group she is spearheading to equip survivors with the tools, training, and support needed to engage lawmakers and advance policies that improve outcomes for patients and families. Sign up here.
During the following Advancing Patient Advocate Voices panel, moderated by Citseko Staples Miller of FTI Consulting, with Matthew, Kate, and Taylor Hosier, Director of Patient Navigation for the Ulman Foundation, the panelists examined how patient advocacy shapes cancer systems and why cross-sector collaboration is essential to lasting change. As Citseko emphasized, “Patients are not an afterthought—they are stakeholders.”

Holding Space for the Full Survivor Experience
The Summit made room for honesty—not just about prevention and policy, but about survivorship itself.
In a heart-centered session, motivational speaker Dr. Stephanie Broadnax Broussard, LCSW-S, APHSW-C, named what many survivors carry quietly: Grief exists alongside survival. Placing a hand over her chest, she reminded the room that grief “exists here,” within the body and the lived experience of being human: chronic pain, neuropathy, changes in identity, intimacy, fertility, and confidence in the future. Community, she said, doesn’t remove grief, but it can help carry it.

That candor carried into Dr. Stephanie’s “Both/And Reality” exercise, inviting survivors and advocates to name two truths they were holding at the same time. The responses captured the complexity of the task in minimal words:
“Grateful and grieving.” – Yvette Torres, Cervivor Ambassador
“Healing and hurting.” – Carol Lacey, Lead Cervivor Ambassador
“Exhausted and resilient.” – Linda Eckert, ObGyn professor and book author

From there, Team Cervivor’s Christina Turpin led an interactive session reminding attendees that while this work is a marathon, the Summit itself was a sprint—an opportunity to capture momentum and turn it into action. Joining virtually, Cervivor community member Leanne offered a simple but resonant affirmation: “I am the positive ripple.”
The Summit’s final speaker was Beth Battaglino, RN-C, CEO of HealthyWomen, whose remarks cut directly to the heart of the moment. “We have the science, we have the tools—and yet,” she said, “every year in the U.S., more than 13,000 people are diagnosed with cervical cancer, and over 4,000 still lose their lives.”

“The gap between what we know and what we do is where your voice matters,” Battaglino continued. Education, she reminded the audience, “doesn’t move on its own. Policy does not change on its own, and access doesn’t expand on its own. People move them forward.”
To close the Summit on a heartfelt note (well, several notes), Cervivor Ambassador and New York music teacher Yvette Torres took the stage to sing the room out with a live rendition of “We Are Cervivor,” a song she wrote and recorded to uplift the cervical cancer survivor community.

Our Heartfelt Thanks—And the Work Continues
To everyone who joined us in Washington, D.C., or followed along online, we offer our sincere gratitude for another successful Summit. A special thank you to our presenting sponsor, Hologic; partnering sponsor, Roche; supporting sponsor, Merck; and our valued in-kind partner, St. Jude HPV Cancer Prevention Program.
We are also deeply grateful to our exhibitors, who made the Summit even more enriching for attendees. We appreciate all that they brought (literally!) to the event: the National Foundation for Infectious Diseases (NFID), Ulman Foundation, Hopewell Cancer Support, ACHIEVE (The ACHIEVE Study), and KickIt Pajamas, co-founded by Cervivor Ambassador Cindy Trice. As always, we thank our dedicated volunteers who made this Summit possible.
But, as Cervivor’s founder Tamika reminded attendees at the outset, the work doesn’t end with the Summit. The 2026 Cervical Cancer Summit reaffirmed what Cervivor has known for 21 years: We have the data, lived experience, community, and a clear understanding of what works. Ending cervical cancer now requires sustained investment in prevention, survivor leadership, and community-rooted action.

As Cervivor marks 21 years of impact, the Tell 21, Give 21 campaign supports survivor education, advocacy, research engagement, and prevention efforts. It saves lives every day.
We’re grateful to have already surpassed $30,000 toward our goal, and there is still more to do.
Tell your story.
Support the work.
Share the mission.
Together, we can continue building a future where cervical cancer is prevented—and survivors are heard. Save the date for the 2027 Summit!

All images courtesy of Portia Wiggins Photography.
About the Author

SARA LYLE-INGERSOLL is a seasoned content and communications expert dedicated to transforming lived experiences into impactful stories. Her award-winning magazine feature about a close friend who passed from cervical cancer in their twenties led her to connect with Cervivor’s founder, Tamika Felder, and solidified her commitment to cervical cancer awareness and prevention. Now, as Cervivor’s Communications Director, Sara brings this mission full circle.