Happy 50th Birthday to our Founder, Chief Visionary, and Global Trailblazer, Tamika Felder!
Today, we don’t just celebrate a birthday — we celebrate a legacy in motion.

Diagnosed with cervical cancer at just 25 years old, Tamika Felder could have let that diagnosis define her limits. Instead, she transformed it into a launching point. What began as one woman’s journey of survivorship has become a global movement centered on advocacy, education, and community.
In 2005, Tamika founded Cervivor, Inc. to create what she wished she had during treatment — a space to be seen, heard, and supported. Her vision gave birth to a powerful community where cervical cancer patients and survivors could raise their voices, share their stories, and make a difference in the lives of others.
Nearly two decades later, Cervivor is now a recognized global leader in the mission to eliminate cervical cancer. And Tamika — still at the helm — remains one of the most influential voices in the cancer advocacy space.
“Every birthday is a big deal when you’ve had cancer, but this one isn’t just about turning 50. It’s about asking: ‘What have I done with this time? What mark have I left?’For me, that answer is Cervivor. Twenty years ago, I founded the organization to create the kind of support I didn’t have: a community where cervical cancer patients and survivors can find their voice, share their stories, and educate others. I’m proud of what we’ve built. We’ve turned pain into power. We’ve built a movement.”


But her impact reaches far beyond this organization. She has:
- Testified before the FDA to ensure patient experiences shape policy.
- Co-chairs the National HPV Vaccination Roundtable, where she advances equitable access to prevention.
- And in 2024, she was appointed to the National Cancer Advisory Board, helping to guide national strategy around research, equity, and care.
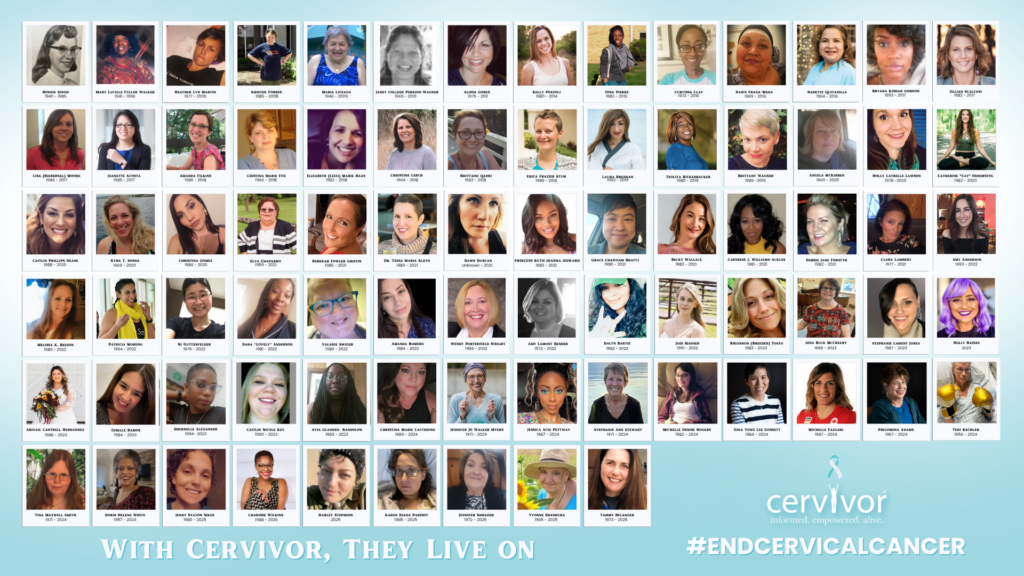
Tamika’s work has transformed systems, shattered stigma, and created space for countless others to rise in their purpose.
The Cervivor Community Reflects
Tamika, your mark is undeniable. You’ve opened doors for others to walk through. You’ve transformed individual stories into collective progress. You’ve given power back to people who never thought they’d be seen.
Tamika’s impact isn’t just professional — it’s deeply personal. The Cervivor community, made up of those whose lives have been touched by her work, shares their heartfelt thanks:

“I know I say this often, but I truly am grateful for you being bold enough to walk in your purpose. You continue to open doors for all of us to walk through. Your reach is immeasurable. Merci beaucoup, Tamika Felder!” — Cervivor Community Member
“You have given so many of us a platform of hope, all while empowering us to use our stories, our voices to create a better tomorrow. Thank you for being unstoppable!” — Cervivor Community Member
“Tamika, you have changed the face of cervical cancer and helped to spotlight the lives and stories of too many patients and survivors to count. I am glad to celebrate you today!” — Cervivor Community Member
“Thank you for everything you do every day to end cervical cancer. You are a force of change and so very needed!” — Cervivor Community Member
Join the Celebration: Honor Her Legacy.
As we reflect on Tamika’s 24 years of global impact, we’re reminded of the power of resilience and determination. From creating a community for those affected by cervical cancer to advocating for awareness, education, and research, Tamika’s work has changed lives and saved lives.

Through Cervivor, Inc., she has given a voice to the voiceless, hope to the hopeless, and support to those navigating the complexities of cervical cancer. Her legacy is a testament to transformation through adversity and turning it into purpose.
Tamika’s story is one of courage, perseverance, and compassion, inspiring a movement that continues to grow and evolve.
As Cervivor, Inc. stands strong today, it’s a direct result of Tamika’s vision, leadership, and commitment to eliminating cervical cancer once and for all. Now, it’s our turn to celebrate her legacy.
In honor of her 50th birthday:
- Share — how Tamika’s work has inspired or impacted you.
- Give to support Cervivor’s work — because access, education, and advocacy save lives.
- Get involved — share your story, raise awareness, and be part of the change.
- Use your voice — because your story matters, and together we can eliminate cervical cancer.
Let’s show Tamika and the world that her impact has not only mattered, but multiplied. Happy 50th Birthday, Tamika Felder. Your legacy is powerful. Your leadership is transformative. Your voice has changed the world.